BRIEF HISTORY
A man of 47 was admitted with a three-hour history of central chest pain and shortness of breath. His pain radiated to the left shoulder and lower jaw and was moderate-to-severe in intensity. He was diagnosed to have exertional angina three months ago and was advised to lose weight and take angised tablets as required. He had been tried 3 such tablets before coming to the hospital but with no relief. He had been attending a wedding party and ate heavy meals night before and thought the pain might have been due to indigestion, therefore, he had also tried some antacids, but this did not help the pain either. He had felt nauseated in the last two hours and had profuse, cold sweating on the forehead. He had been fit and healthy until three months ago. He lived with his wife, had two sons, 18-and-16-years old. He had been smoking 25 cigarettes a day for over 25 years until three months ago when he stopped smoking on his doctor’s advice. His father died at the age of 53, his mother was 68 and healthy and one brother, 51 was also in good health.
IMPORTANT CLUES ON CLINICAL EXAMINATION
On examination, he was obese, JVP was not raised. Blood pressure was 130/70 mmHg. Pulse was 68 per minute with occasional extrasystoles. Respiration was 20 per minute. There was no cyanosis, thyroid enlargement or lymphadenopathy. Heart sounds were normal. He had a soft, systolic, apical murmur with no radiation. Trachea was central. Breath sounds were normal with a few left basal crepitations. Examination of abdomen and central nervous system was normal.
DETERIORATION ON THE THIRD DAY OR FURTHER FOLLOW UP
His condition improved after treatment with morphine, oxygen and bed rest. However, on the third day, he suddenly became dyspnoeic and complained of tightness in his chest. His blood pressure dropped to 90/50 mmHg, pulse was 40 per minute and respiratory rate was 34 per minute. On examination at this stage, he was found to have developed a pansystolic apical murmur radiating to the left axilla. There was no evidence of deep vein thrombosis in the legs. His chest was full of crackles bilaterally. Examination of central nervous system and abdomen remained unremarkable.
QUESTIONS
Q.1.
What is the most likely cause of this patients deterioration on the third day of his admission?
Q.2.
How could you explain the pan-systolic murmur and what treatment could be offered?
Q.3.
What happened on the third day?
Q.4. Name six complications of your diagnosed disease which may be seen within the first week.
Q.5.
How would you clinically diagnose complete heart block?
Q.6.
What is the role of streptokinase and tissue plasminogen activator (tPA)?
A.1.
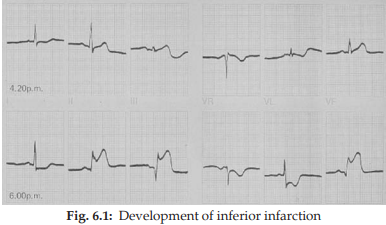
Initial diagnosis in this forty-seven year old obese gentleman with history of smoking and family history of heart disease with recently diagnosed angina is ischaemic heart disease. But the onset of severe chest pain radiating to jaw and associated with sweating indicate an acute myocardial infarction. Papillary muscle rupture is not an uncommon complication in the first week and typically presents with signs of shock and left ventricular failure. The sudden appearance of pan systolic apical murmur, falling blood pressure, pulmonary congestion and tachypnoea are suggestive of this complication.
A.2.
Papillary muscle rupture explains the pan-systolic murmur. It requires immediate assessment and treatment with: i. Morphine ii. Oxygen iii. Digoxin iv. Inotropic support to increase the blood pressure adequately. v. Consider surgical intervention in cases of failure of medical therapy. Intra-aortic balloon pump may be required till surgery is arranged.
A.3.
The patient dropped his blood pressure and had bradycardia which indicated that he had developed complete heart block. He had also developed a new pansystolic apical murmur suggestive of papillary muscle rupture.
A.4.
i. Various cardiac arrhythmias
ii. Cardiogenic shock
iii. Congestive cardiac failure
iv. Pericarditis
v. Rupture of interventricular septum, chordae tendinae or the myocardium.
vi. Thrombo-embolism—systemic or pulmonary.
A.5.
Clinically at the bed side, complete heart block can be recognised by: i. Marked bradycardia, i.e, less than 40 beats/minute
ii. Low blood pressure
iii. Loud and variable 1st heart sound
iv. Cannon waves (giant “ a “ wave) in the jugular venous pressure.
A.6.
Streptokinase, which is an enzyme derived from microorganisms, if given in the first four hours of the onset of pain, produces very good results both clinically and electrocardiographically. Usual dose is 1.5 million units diluted in 100 c.c. of N. saline and infused over an hour. Tissue plasminogen activator (tPA) is better than streptokinase but is much more expensive. The dose is usually 10 mg IV start, then 50 mg over 1 hour then 40 mg over next two hours. Results are better than streptokinase.
need an explanation for this answer? contact us directly to get an explanation for this answer