A 55-year-old male develops complaints of sudden onset persistent diplopia while looking ahead since a week. On questioning, he lets us know that he has had similar complaints of diplopia intermittently, especially on waking up for the last two months which did not interfere with his daily activities. He has also noticed complaints of redness in the right eye and a feeling of grittiness in both eyes. His wife adds that it seems like his eyes are ‘popping out’ of his sockets. He has noticed weight loss of around 8% over the last few months with insomnia and fatigue, both of which he attributed to his current change of his boss at work and hence was not investigated for. His sister has primary hypothyroidism and is on levothyroxine supplements. He is a smoker (20 pack years). On examination, he is well built, with a BMI of 26 kg/m2. He appeared anxious, has a pulse rate of 100 bpm, blood pressure of 150/90 mm Hg, warm moist palms, has fine tremors of extremities and a diffuse goiter with no bruit. Eye examination reveals proptosis both eyes (R > L). Lateral movement of the right eye is restricted to 30° from midposition. Clinical activity score was right eye 4/7 (conjunctival redness, pain on movement, chemosis and swelling of the eyelids and the left eye 3/7 (pain on movement,conjunctival redness and chemosis). No dermopathy or nail changes noticed.
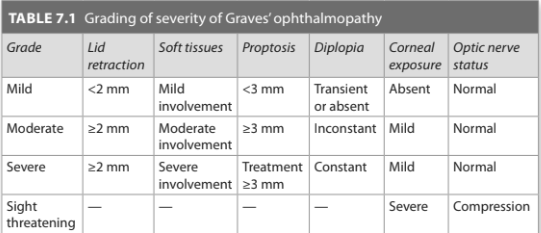
Investigations revealed a normal hemogram with normal total and differential leukocyte count. TSH <0.001 μIU/mL, free T4 80 ng/dL. Technetium uptake scan shows diffuse increased uptake over the entire gland. A diagnosis of Graves’ disease with moderate-to-severe, clinically active ophthalmopathy is made.
How is active, moderate-to-severe ophthalmopathy managed?
This group of patients qualify for glucocorticoids to bring down the activity
of the disease. Intravenous glucocorticoids pulses have higher response rates as compared to oral glucocorticoids. Various regimens are used. One of them is 500 mg IV pulses three consecutive days, repeated in 4 monthly cycles with a cumulative dose of 6 g. Higher cumulative doses of IV steroids increase the risk of acute liver injury.
Oral steroids (Prednisolone @ 1 mg/kg/day) also can be initiated for 4–6 weeks and tapered over the next 4 weeks. Ophthalmopathy may flare up on attempts to withdraw steroids. Screening for conditions that can worsen with steroid therapy is imperative. Bone protection in the form adequate calcium and vitamin D supplementation with or without bisphosphonates are to be provided.
need an explanation for this answer? contact us directly to get an explanation for this answer