A 55-year-old male develops complaints of sudden onset persistent diplopia while looking ahead since a week. On questioning, he lets us know that he has had similar complaints of diplopia intermittently, especially on waking up for the last two months which did not interfere with his daily activities. He has also noticed complaints of redness in the right eye and a feeling of grittiness in both eyes. His wife adds that it seems like his eyes are ‘popping out’ of his sockets. He has noticed weight loss of around 8% over the last few months with insomnia and fatigue, both of which he attributed to his current change of his boss at work and hence was not investigated for. His sister has primary hypothyroidism and is on levothyroxine supplements. He is a smoker (20 pack years). On examination, he is well built, with a BMI of 26 kg/m2. He appeared anxious, has a pulse rate of 100 bpm, blood pressure of 150/90 mm Hg, warm moist palms, has fine tremors of extremities and a diffuse goiter with no bruit. Eye examination reveals proptosis both eyes (R > L). Lateral movement of the right eye is restricted to 30° from midposition. Clinical activity score was right eye 4/7 (conjunctival redness, pain on movement, chemosis and swelling of the eyelids and the left eye 3/7 (pain on movement,conjunctival redness and chemosis). No dermopathy or nail changes noticed.
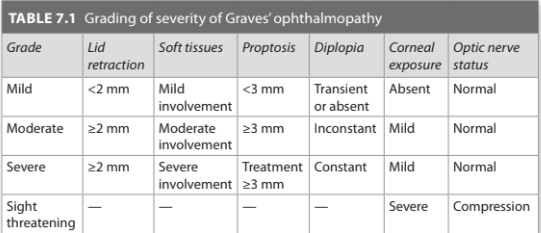
Investigations revealed a normal hemogram with normal total and differential leukocyte count. TSH <0.001 μIU/mL, free T4 80 ng/dL. Technetium uptake scan shows diffuse increased uptake over the entire gland. A diagnosis of Graves’ disease with moderate-to-severe, clinically active ophthalmopathy is made.
How is sight-threatening ophthalmopathy managed?
At every follow-up visit, patients need to be asked specifically about a decrease in visual acuity and tested for visual acuity as well. If a drop is noted, urgent referral to an ophthalmologist is to be made to assess visual fields, relative afferent papillary defect and color vision. If dysthyroid optic neuropathy is diagnosed, the patient warrants high dose intravenous glucocorticoids. If no improvements are seen, in a 1–2 weeks time, orbital decompression surgery is to be undertaken.
The second form of sight-threatening ophthalmopathy is corneal breakdown/ ulceration. The role of steroids on corneal breakdown is unknown. Hourly lubrication of the eye, temporary methods to decrease exposure of cornea-like tarsorrhaphy, moisture chamber, or botulinum toxin injection can be tried while orbital decompression is planned at the earliest.
need an explanation for this answer? contact us directly to get an explanation for this answer