A 67-year-old male is referred by h is primary care physician for further evaluation of elevated hemoglobi n level. Patien t reports feeling generally wel l; however. on review of systems. he does report mild fatigue and left abdominal discomfort. Patien t is a non-smoker with no h istory of cardiac or pulmonary disease. Exami nation reveals a male with a ruddy complexion and splenomegaly. Laboratory workup shows hemoglobin of 1 9 .5 g/dl. mean corpuscu lar volume 79 FL. leukocyte count of 1 9 .800/JLL. and plate-let count of 3 56.000/JLL. Peripheral blood smear shows no gross abnormalities. Testing for JAK2 V6 1 7 F mutation is instead of returned positive. and patien t is diagnosed with polycythemia vera (PV) .
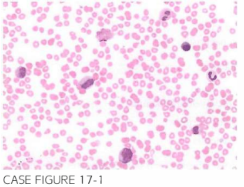
Patien t is treated appropriately and is followed for the next 9 years until he notes pro-gressive i ncrease in his abdominal girth and fatigue. Physical examination reveals in-creased splenomegaly. Hemoglobin level is found to be 8.7 g/dl. leukocyte count 9,800/JLL. and platelets count 1 1 5 .000/JLL. Peripheral blood smear is shown below.
What is the most likely explanation of patient's presentation?
- Splenic vein thrombosis
- Budd Chiari syndrome
- Transformation to acute leukemia
- Transformation to myelofibrosis
- Chronic gastrointestinal bleeding
D. Peripheral blood smear reveals abnormal teardrop-shaped red blood cells, nucleated red blood cells, and promyelocytes. There is no evidence of blasts. This picture is most consistent with progression to post-PV myelofibrosis. Progression to post-PV myelofibrosis has been reported with a frequency of 16% at 10 years and 34% at 15 years of follow-up (Br J Haematol. 2009;146(5):504).
need an explanation for this answer? contact us directly to get an explanation for this answer