History
A 27-year-old woman attends the antenatal clinic at 19 weeks’ gestation in her first ongoing pregnancy, having had a termination aged 22 years. She is now happy to be pregnant. She booked with the midwife at 8 weeks and has had normal booking bloods, blood pressure and ultrasound scan. She experienced nausea and vomiting until 14 weeks’ gestation. This has now settled but she remains very tired and feels that she is gaining excessive weight in the pregnancy. She also feels cold for much of the time, which surprises her as she understood that pregnant women tend to feel hot.
Examination
The woman appears lethargic and of low mood. Her blood pressure is 115/68 mmHg and heart rate 58/min. Abdominal examination is unremarkable, with the fundus palpable at the umbilicus.
Questions
• What is the diagnosis and what features will you look for on examination?
• What are the implications for the mother and baby in pregnancy?
• How should the condition be managed?
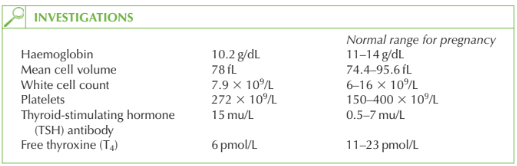
The full blood count shows mild anaemia, with relatively low mean cell volume. This is not significant enough to account for the symptoms described. The thyroid function tests confirm the clinical diagnosis of hypothyroidism. There is no history of radioactive iodine or surgical treatment, and Hashimoto’s thyroiditis is unlikely as there has been no history of a hyperthyroid episode. This case therefore probably represents idiopathic myxoedema. The symptoms of tiredness, cold intolerance and weight gain may all relate to the hypo-thyroidism. In addition she may report dry skin, coarse hair, depression or constipation.
Examination may reveal relative bradycardia, blunted deep tendon reflexes or goitre. Implications for the pregnancy and management Hypothyroidism occurs in approximately 1 in 100 pregnancies, but this case is unusual to be diagnosed in pregnancy.
Myxoedematous coma is a very rare consequence of hypothyroidism, associated with a high mortality rate. It is a medical emergency managed by supportive care and thyroxine supplementation. In the absence of a coma, thyroxine replacement is still needed and should be titrated to the TSH and T4 results.
In pregnancy, the thyroxine requirement may increase, and the TSH and T4 should be checked every trimester once a maintenance regime has been established. The aim should be to keep the TSH less than 5 mu/L. (Although the thyroid-binding globulin increases in pregnancy, there is a compensatory rise in tri-iodothyronine (T3) and T4 production such that the levels of free T3 and free T4remain similar to non-pregnant values.)
The fetus
Untreated hypothyroidism is associated with an increased risk of infertility, miscarriage, stillbirth and pre-eclampsia. The fetal and neonatal outcome is generally good in women diagnosed and treated appropriately. Anti-TSH antibodies may very rarely cross the pla- centa and cause neonatal hypothyroidism, and this should be suspected if there are signs of neonatal goitre.
KEY POINTS
• Untreated hypothyroidism is associated with infertility, miscarriage, low birth weight, fetal loss, pre-eclampsia and anaemia.
• Women established on thyroxine should have thyroid function monitored once in each trimester of pregnancy.
need an explanation for this answer? contact us directly to get an explanation for this answer