History
A 24-year-old student is referred to the gynaecologist on call from the emergency depart- ment with sudden-onset of left iliac fossa pain which woke her at 2 am. She fell asleep again but since 8 am the pain has been constant and is not relieved by ibuprofen or cody-dramol. Her last period started 2 weeks ago and she reports no irregular bleeding or discharge. She has no significant gynaecological history except for a termination of pregnancy age 17 years. She has been with her current boyfriend for 2 years and has used the combined oral contraceptive pill (COCP) throughout that time. She says she has not had intercourse for the last 4 months because her boyfriend has been travelling, but says that intercourse has never been painful. On direct questioning she has felt nauseated but has not vomited. She has had no urinary symptoms but has opened her bowels several times each day for the last 3 days, which is unusual for her.
Examination
On examination she is apyrexial, her observations are normal and her abdomen is soft with vague left iliac fossa tenderness but no signs of peritonism. Bimanual examination reveals a normal-sized uterus with no adnexal tenderness or cervical excitation and non obvious adnexal masses.
Questions
• What is the first investigation you would like to perform?
• What is your differential diagnosis if this test is negative, and how would you rule out some of these diagnoses?
Any woman of reproductive age with abdominal pain should always have a urinary preg-nancy test, regardless of the date of her last menstrual period. In this case the test is nnegative.
The remaining differential diagnoses include:
• ovarian cyst
• pelvic inflammatory disease
• urinary tract infection or stone
• bowel-related cause.
There are no specific gynaecological symptoms or adnexal tenderness, which implies that the pain is not gynaecological in origin. However, during speculum examination it is pru-dent to send swabs for chlamydial and gonorrhoeal infection opportunistically, in view of the high background prevalence of sexually transmitted infection, especially in the 18–25-year-old age group. Ovulation pain (mittelschmirtz) or a corpus luteal cyst are very unlikely as the COCP inhibits the ovulatory cycle. However, a transvaginal ultrasound scan will rule out an ovarian cyst for certain. Urine should be dipped for blood to rule out a renal stone, and for leucocytes and nitrites to rule out infection.
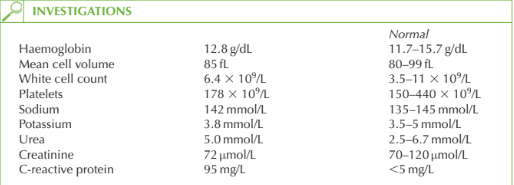
Bowel habit is altered and the raised C-reactive protein suggests an inflammatory condi-tion. As the onset is acute and not severe, the diagnosis is likely to be gastroenteritis. This should be managed expectantly, with fluids, rest and simple analgesia. A stool culture should be sent if the symptoms fail to resolve. Other inflammatory bowel conditions such as Crohn’s disease and ulcerative colitis are rare causes to consider if the symptoms are persistent or recurrent.
Irritable bowel syndrome is not associated with raised inflammatory markers, and is there-fore not a differential diagnosis in this case.
KEY POINTS
• Gynaecological, urinary and bowel-related pathology can all be associated with lower abdominal pain.
• A thorough and focused history is always important in making a correct diagnosis.
need an explanation for this answer? contact us directly to get an explanation for this answer