History
A 24-year-old woman presents with pelvic pain and painful sexual intercourse for 2 years and is worried that she may have an ovarian cyst or other gynaecological problem. The pain occurs at any time of the menstrual cycle but is worse during menstruation. It can also be worse when she passes urine or opens her bowels. There is no relation to exercise. She has been with her current sexual partner for 6 months and the pain occurs nearly every time she has intercourse unless penetration is very gentle. She has never been diag-nosed with any sexually transmitted infections. She has been pregnant once at the age of 19 years but this ended in a spontaneous complete miscarriage. She opens her bowels regularly and denies any bloating, constipation, diarrhoea or mucus in the stool. She had an episode of cystitis a few years ago which responded to antibiotics. There is no other medical history of note and she takes no regular medications.
Examination
The abdomen is not distended and there is no organomegaly. No masses are palpable but there is suprapubic tenderness. Speculum examination shows a normal smooth grey/white coloured discharge and swabs are taken. The uterus is anteverted but has limited mobility and is tender on movement. There are no adnexal masses but the adnexae are tender.

Questions
• What is the diagnosis?
• How would you manage this patient?
• What are the long-term implications of this disease?
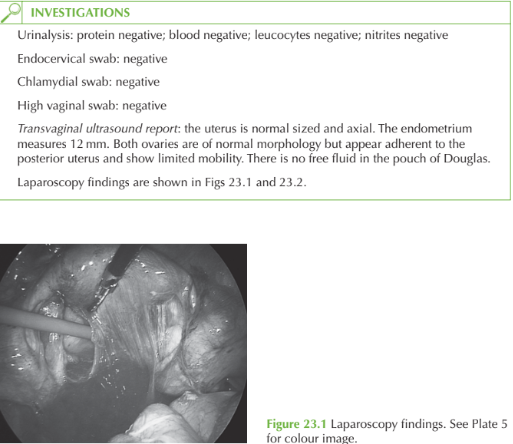
The laparoscopy image shows in Fig. 23.1 pelvic adhesions suggestive of previous infec-tion. The ‘violin-string’ perihepatic adhesions in Fig. 23.2 are classical of Fitz-Hugh–Curtis syndrome, generally seen with previous chlamydial infection though also described with gonorrhoea. These findings can develop in the absence of a clinically recognized infective episode. bThe woman therefore has chronic pain from pelvic inflammatory disease. Negative swabs would suggest that she may no longer be infected with chlamydia.
Management
The pain may be helped with laparoscopic adhesiolysis. The perihepatic adhesions should be ignored as they are not causing symptoms. Otherwise pain-management options are analgesics or possible uterosacral nerve ablation. Even though there is no evidence of current active infection, the tests have limited sensi-tivity so it is worthwhile treating the woman and her partner with a course of antibiotics for pelvic inflammatory disease.
KEY POINTS
• Fitz-Hugh–Curtis syndrome is the presence of perihepatic adhesions in association with previous chlamydial or gonococcal infection.
• Treatment of both partners is appropriate.
• Chronic pain, ectopic pregnancy and tubal infertility are long-term consequences of pelvic inflammatory disease.
need an explanation for this answer? contact us directly to get an explanation for this answer