History
A 61-year-old woman complains of involuntary loss of urine. She has noticed it gradually over the last 10 years and has finally decided to see her general practitioner about it after hearing a programme on the radio about treatment for incontinence. The leaking is gen-erally small amounts and she wears a pad all the time. It tends to occur when she cannot get to the toilet in time. She never leaks on coughing or sneezing. She suffers urgency, particularly when she comes home after being out and is about to come into the house.
She also has frequency, passing urine every hour during the day and getting up two or three times each night. Due to the incontinence she tries not to drink much and usually has two cups of tea first thing in the morning, coffee mid-morning and a further cup of tea mid-afternoon. Other than that she drinks one glass of squash per day and has one glass of wine at night. She is a non-smoker. She has had two uncomplicated vaginal deliveries. Her periods stopped at the age of 54 years. There is no other gynaecological or medical history of note.
Examination
Abdominal examination is normal. On vaginal examination there is minimal uterovaginal descent and no anterior or posterior vaginal wall prolapse.
Questions
• What is the diagnosis?
• How would you advise and manage this patient?
The diagnosis is of overactive bladder syndrome (OAB). This was formerly referred to as detrusor instability. In this condition the bladder contracts involuntarily without the nor-mal trigger to void caused by bladder filling. This results in involuntary loss of urine that is embarrassing and often impacts enormously on women’s lives, as they are constantly aware of needing to void and where the nearest toilet might be.
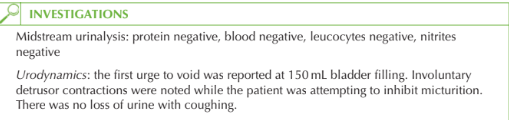
Urodynamic investigation with filling and voiding cystometry is helpful (as in this case) in confirming the diagnosis by showing spontaneous detrusor contractions during blad- der filling.
It is important to exclude other causes of such symptoms (such as urinary tract infection or a bladder tumour) with urine microscopy.
Management
• Conservative:
• the woman should be advised that both caffeine and alcohol are bladder stimulants and are likely to worsen symptoms so should be minimized. She should take a nor-mal fluid intake per day but avoid drinks after about 7 pm to limit nocturia
• bladder retraining for 6 weeks, involving a ‘drill’ restricting voiding to increasing intervals should be taught.
• Medical treatment: if lifestyle advice and bladder retraining fail then anticholinergic medication such as oxybutynin or tolterodine should be commenced. The associated side-effects include dry mouth, dry eyes and constipation.
KEY POINTS
• Overactive bladder syndrome is associated with urgency, frequency and urge incontinence.
• Conservative measures are bladder retraining and caffeine avoidance.
• Medical treatment is with anticholinergics.
need an explanation for this answer? contact us directly to get an explanation for this answer