History
A 43-year-old woman is referred from her general practitioner (GP) with painful periods. She says that her periods have always been quite heavy and painful but that in the last 2–3 years they have become almost unbearable. She bleeds every 24 days and the period lasts for 7–9 days with very heavy flow from day 2 to day 6. The pain starts approximately 36 h before the onset of the bleeding and lasts until about day 5. The pain is constant, dull and severe, such that she cannot do any housework or any social activities during this time. Her GP has prescribed paracetamol and mefenamic acid in combination, which she says ‘takes the edge off’ but does not fully relieve the symptoms. She has had four normal deliveries and her husband had a vasectomy several years ago. There is no history of intermenstrual or postcoital discharge and she has no abnormal dis-charge. Her smear history is normal, the most recent being 18 months ago. She takes citalopram for depression but currently reports her mood as fine. She does not drink alco-hol or smoke.
Examination
The abdomen is soft and there is vague tenderness in the suprapubic area. The cervix appears normal. On bimanual palpation the uterus is approximately 10 weeks size, soft and bulky. She is tender on palpation but there is no cervical excitation, adnexal tender-ness or adnexal masses.
Questions
• What is the likely diagnosis?
• How would you further investigate and manage this woman?
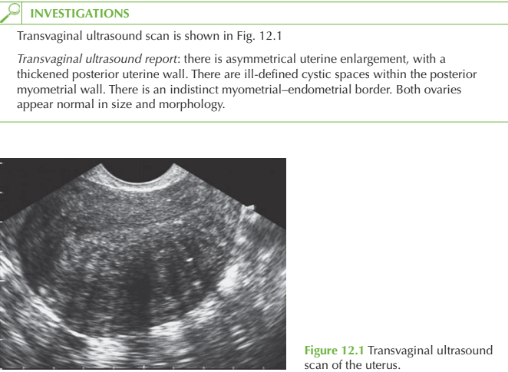
The symptoms of dysmenorrhoea and menorrhagia and the ultrasound report suggest a diag- nosis of adenomyosis. This is a benign condition whereby functioning endometrial glands and stroma are found within the myometrium. With each period bleeding occurs from the endometrial tissue into the smooth muscle, with associated pain. It tends to occur in women over 35 years and risk factors include increased parity, termination and previous Caesarean section. The condition may commonly be found in association with endometriosis. Classically the diagnosis may only be made histologically after hysterec-tomy for dysmenorrhoea. More recently however the diagnosis can be suspected by ultra-sound or magnetic resonance imaging (MRI) scan.
Further investigation If the diagnosis is in doubt then an MRI scan may be requested. Hysterectomy to obtain histological diagnosis would be inappropriate.
Management
The initial management involves analgesia such as mefenamic acid and codydramol. Tranexamic acid reduces the amount of bleeding and this may secondarily reduce the amount of pain. Suppression of menstruation with gonadotrophin-releasing hormone analogues is a short-term measure. The levonorgestrel-releasing intrauterine device is another option to locally suppress the endometrial tissue, and may resolve the pain. As a last resort hysterectomy should be performed.
KEY POINTS
• The prevalence of adenomyosis is unknown, as diagnosis is only confirmed by hysterectomy.
• It is a cause of menorrhagia and dysmenorrhoea in older women.
• Hysterectomy may be avoided by use of analgesia or hormonal suppression.
need an explanation for this answer? contact us directly to get an explanation for this answer