History
A dermatology opinion is sought for a 47-year-old in-patient on the haematology ward.He has noticed slowly progressive redness and scaling of his feet and left palm, which is minimally itchy. In addition he has extensive discolouration and brittleness of his toenails and fingernails of the left hand. He had first noticed the skin and nail changes 4 months previously. There is no family or personal history of skin/nail problems. He is currently an in-patient, having undergone an autologous stem cell transplantation for multiple myeloma associated with systemic amyloidosis. Prior to the transplant he had been receiving high-dose melphalan.
Examination
The skin on the soles of his feet and left palm is erythematous with scaling and desqua-mation. Nail plates are dystrophic and brittle distally, Beau’s lines are evident (horizontal indentation of the nail plates) and there is associated periungal erythema (Fig. 87.1).

Questions
• What is the likely cause of the skin and nail abnormalities?
• What treatment could be offered?
Skin scaling on the hand/foot and nail dystrophy can be associated with palmar–plantar psoriasis, severe pompholyx eczema, or dermatophyte (fungal) infections. As a gen-eral rule cutaneous inflammatory disorders are more likely to present in a symmetrical
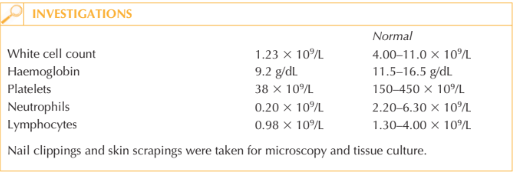
fashion than infections. This patient had been receiving chemotherapy and a stem cell transplantation, and therefore had undergone a prolonged period of immunosuppression, which had left him vulnerable to infections. Nail clippings and skin scrapings were sent for mycological analysis. Fungal hyphae were seen on microscopy and cultures from skin and nails grew Trichophyton rubrum. Dermatophyte fungi invade the epidermis and keratinized tissues of the skin, nails and hair. Adults are more susceptible than children to tinea pedis (athlete’s foot) and ony- chomycosis (fungal nail infection). It is estimated that about 3–8 per cent of the adult population is affected by onychomycosis. In diabetic patients and those who are immu-nosuppressed the incidence is higher.
Invasion of the nail plate distally and laterally usually follows chronic tinea pedis. As fungi penetrate through the nail plate it lifts up off the nail bed – so-called onycholysis. The nail plate itself becomes brittle, discoloured and may become hyperkeratotic. The most common fungi implicated in onychomycosis in Europe include T. rubrum, T. inter-digitale, T. tonsurans and Candida albicans. Treatment of onychomycosis is guided by the severity, symptoms, number of nails affected, possible drug interactions, drug intolerance and patient expectation. Choosing the right antifungal preparation is aided by the identification of the underlying causa-tive fungus. Dermatophyte fungi including Trichophyton spp. can be treated with oral terbinafine (6-12 weeks) or itraconazole (continuous or pulsed for 3–4 months). Topical preparations (applied twice weekly for 6-12 months) are usually reserved for more limited nail disease or for those unable to take oral antifungal drugs.
Candida yeast around the nails is usually present in a mixed infection along with dermatophyte fungi and/or bacteria. Fluconazole orally can be helpful, as can topical clotrimazole, for any associated Candida skin involvement.
KEY POINTS
• Fungal nail infections are most common amongst adults and immunosuppressed patients.
• Onychomycosis causes morbidity and cosmetic embarrassment rather than severe disease.
• Oral antifungal drugs are more effective than topical treatment alone in treating nychomycosis.
need an explanation for this answer? contact us directly to get an explanation for this answer