History
A 37-year-old healthcare assistant presents to the dermatology clinic with a pruritic erup-tion over her right knee. The lesion had started as a small erythematous papule and then spread out very gradually to form a scaly, ring-shaped lesion. The itching is not intense but she does find herself scratching. She has no history of previous skin problems. Her 7-year-old son has eczema and a dry scaly scalp. She has used some of her son’s cortisone ointment on the lesion, which seemed to reduce the itching and scaling but the lesion has continued to expand.
Examination
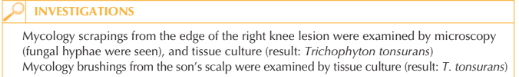
There is an annular lesion 9 cm in diameter with a raised edge over the right knee (Fig. 86.1). Marked hyperpigmentation, erythema and multiple papules and pustules are seen at the raised edge. Her scalp and nails are normal, as is the rest of her skin. She has brought her son with her to the clinic; he has a very scaly scalp with patches of alopecia and occipital lymphadenopathy.

Questions
• What is the diagnosis?
• From whom did the patient acquire the infection?
• How would you treat the mother and child?
The healthcare assistant has a cutaneous fungal infection caused by the dermatophyte Trichophyton tonsurans. The patient had used a cortisone ointment on the fungal infection which altered the cutaneous appearance. This phenomenon is so-called ‘tinea incognito’ (steroid-modified tinea), whereby the fungal infection continues to spread outwards but the scale is reduced and small papules and pustules may appear at the growing margin.
T. tonsurans is the main cause of tinea capitis (scalp ‘ringworm’) in children living in urban areas.
The fungus is anthropophilic – that is, passed between humans. The usual cutaneous manifesta-tion of tinea corporis (i.e. not treated with topical corticosteroid) is shown in Figure 86.2. The classic presentation includes annular lesions that are scaly at the edge with central clearing; the eruption is mildly pruritic.
The patient’s son had tinea capitis, which is the most likely source of the infection. T. tonsurans is likely to spread to adults when the infected child’s head comes into direct contact with the adults’ skin, usually on the neck / anterior chest where a child’s head rests whilst sitting on their lap. If an adult presents with a T. tonsurans, ask about contact with children.
Samples for mycology are very easy to take and results are useful in guiding treatment. Skin scrapings can be taken using a blunt scalpel blade from the active edge of the lesions. Samples should be sent to the laboratory in folded coloured paper. Scalp brush-ings can be taken using plastic sterile disposable travel toothbrushes, using brisk brushing movements back and forth across the scalp. Brush siblings and parents.
T. tonsurans is an endothrix fungus, which means that the fungal spores reside inside the hair shaft; consequently, scalp infections need to be managed with systemic antifungal medications. In the past, griseofulvin was used to treat tinea capitis in children at a dose of 10 mg/kg daily for 6–8 weeks, however one month of terbinafine is equally effective and better tolerated at a daily dose depending on the child’s weight: 20 kg, 62.5 mg; 20–40 kg, 125 mg; 40 kg, 250 mg. Tinea corporis can be managed with topical terbin-afine 1% cream used twice daily for 4-6 weeks. Alternatives are oral terbinafine 250 mg daily for 2 weeks or oral itraconazole 400 mg daily for 1 week.
KEY POINTS
• A cutaneous fungal infection should be suspected in a patient with isolated scaly annular lesions.
• Classical signs of tinea can be altered by topical steroid use or secondary bacterial infection.
• Tinea capitis in urban areas is most frequently caused by endothrix fungal species that require systemic therapy.
need an explanation for this answer? contact us directly to get an explanation for this answer