History
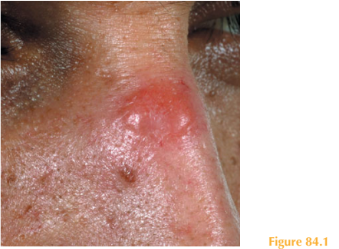
A 28-year-old Turkish Cypriot man came to the United Kingdom to visit relatives for a few months. During his visit he noticed that a small erythematous lesion on his nose was increasing in size and his relatives brought him to the accident and emergency department.
He is referred to the dermatology team for an opinion. The lesion is asymptomatic and has been growing slowly over a period of four months. In Cyprus, where he works in the construction industry, he did not recall any history of trauma to the affected area during his work. He does not burn in the sun and is tanned relatively easily. He is otherwise well, and takes no regular medication.
Examination
There is an erythematous nodule at the root of the nose; the overlying epidermis is nor-mal but there is an indurated swelling in the dermis which is firm on palpation (Fig. 84.1).
There is no ulceration or evidence of telangiectasia within the lesion. Examination of his mucous membranes is normal, there is no regional lymphadenopathy or organomegaly.
He has a BCG vaccination scar on his upper left arm, the rest of his skin check is normal.
Questions
• What is the most likely clinical diagnosis?
• What would you expect the culture and PCR analysis to show?
• How would you manage this patient?
The skin histopathology from the lesion showed ill-defined granulomas with lymphocytes, plasma cells and eosinophils, there was no evidence of vasculitis. Special stains for micro-organisms were negative. The differential diagnoses of cutaneous granulomas include sarcoidosis, tuberculosis, deep fungal infections, leishmaniasis, foreign body reactions, granuloma annulare and granuloma faciale. Microbiological culture from lesional skin grew Leishmania protozoan parasites. PCR confirmed the species Leishmania donovanii complex. The patient was therefore diagnosed with cutaneous leishmaniasis.
There are many different species of Leishmania, each confined to a geographical region of the world and transmitted by the bite of the female sandfly vector. Bites usually occur at night on exposed skin and are not normally painful, therefore patients rarely recall being bitten. Leishmaniasis acquired in Cyprus – so-called ‘old world’ leishmaniasis – can result in cutaneous or mucocutaneous disease.
At the site of the sandfly bite, classically, a small erythematous non-painful papule forms.
Over a few months the lesion increases in size into a nodule that may ulcerate. Localized cutaneous leishmaniasis is usually a self-limiting disease with most lesions healing within 5–15 months. Lesions usually heal with scarring. Treatment aims are to heal lesions more rapidly and try to reduce scarring. In resource-poor settings cryotherapy or heat therapy can be successfully used; however, if available, intra-lesional stibogluconate is highly effective. This pentavalent antimony-containing compound is injected into the lesion at weekly intervals for a few weeks. This patient received five injections over a 6-week period, causing clinical resolution with minimal scarring.
Patients with mucocutaneous or visceral leishmaniasis may be quite unwell with a tem-perature and malaise. Visceral involvement can lead to a depressed bone marrow (anae-mia, leucopenia and thrombocytopenia) and hepatosplenomegaly. Such patients require systemic treatment with intravenous stibogluconate (20–40 days) or intramuscular penta-midine (10 injections given on alternate days) both of which have challenging side-effect profiles. Liposomal amphotericin B (3 mg/kg per day for 5 days plus a further treatment after 1 week) can be effective and is reasonably well tolerated.
KEY POINTS
• Cutaneous leishmaniasis occurs at the site of a sandfly bite, usually on exposed skin.
• Histopathology and culture from involved skin can confirm the diagnosis; however, PCR is highly specific for species identification.
• Identifying the species of Leishmania involved is important as this guides therapy, whether topical or systemic.
need an explanation for this answer? contact us directly to get an explanation for this answer