History
A 69-year-old retired man is referred by his GP to the on-call dermatology registrar with a 1-week history of increasing pain, erythema and blisters on the left side of his face. He is unable to open his left eye. Two days prior to the onset of the cutaneous eruption the patient had complained of pain on swallowing and pain in the left ear and temple area, when he was prescribed flucloxacillin. He has a history of hypertension and is taking amlodipine and simvastatin.
Examination
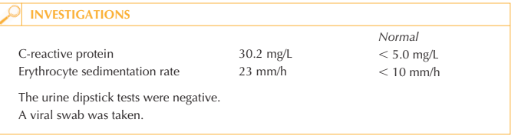
He has marked swelling of the left side of his face with prominent periorbital oedema (Fig. 75.1). There is a sticky discharge around his left eye. He has multiple vesicles on a background of erythema with crusting and erosions. There is a small area of ulceration on the lower lip with multiple ulcers on the hard palate and buccal mucosa. The signs and symptoms are localized to the left side of his face. His temperature is 37.8 oC, blood pressure 133/78 mmHg and pulse rate 67 beats/min.

Questions
• What is the diagnosis?
• What is the source of his infection?
• How would you manage this patient?
This man had herpes zoster virus (HZV) (shingles) affecting the left mandibular branch of the trigeminal nerve. The first symptom is usually tingling followed by severe pain in the skin supplied by the affected nerve. Patients feel unwell and may develop localized tender lymphadenopathy. Within a few days a localized cutaneous eruption occurs in crops of erythematous papules that rapidly form into blisters which then crust over and heal with scarring over a few weeks.
The patient will have acquired HZV from a primary chickenpox infection (usually in childhood) after which the virus remains latent in the spinal dorsal root ganglia. When the virus is reactivated (most frequently in the elderly) as shingles the cutaneous der-matome supplied by the sensory nerve is affected. In this case the mandibular branch of the trigeminal nerve was affected resulting in cutaneous/mucocutaneous signs in the distribution of the nerve (supplying the skin of the temporal region, lower lip and chin, buccal mucosa, muscles of mastication, mucous membrane of the anterior two-thirds of the tongue). Sensory nerve involvement is characteristic of shingles; however, 5 per cent of cases include motor nerve involvement. Multi-dermatomal shingles is seen in immu- nocompromised patients.
If possible, patients should receive aciclovir within 72 hours of the onset of the cutaneous eruption. Oral aciclovir is sufficient for the majority of patients (800 mg five times daily for 7–10 days). However, this patient developed severe oral ulceration and pain on swal-lowing and therefore was treated with intravenous aciclovir (5 mg/kg body weight, three times a day) for the first 48 hours of his treatment followed by a further 7 days of oral therapy. Consider intravenous therapy if there is involvement of the eye, motor nerves or if the patient is immunocompromised. If motor involvement is severe, consider giving oral prednisolone in addition to aciclovir.
The cutaneous eruption should be treated topically with an emollient such as 50:50 white soft paraffin with liquid paraffin (hourly if necessary) to keep the affected skin greasy.
The emollient helps reduce pain in the eroded areas and the likelihood of fissures (skin splitting) as the blisters crust over. The emollient also acts as a barrier to help prevent secondary bacterial infection in the denuded areas of skin. Topical antibiotic ointments may be indicated if secondary infection is suspected. Occasionally oral antibiotics may be indicated.
This patient was jointly managed with the ophthalmologists who recommended regular eyelid cleaning with sterile normal saline and chloramphenicol 1% ointment four times daily to the left eye. Analgesia (such as non-steroidal anti-inflammatory drugs) should be given in the acute phase and for post-herpetic neuralgia, which may be severe and protracted (consider gabapentin or amitriptyline).
KEY POINTS
• Treatment with antiviral drugs should be started as early as possible to improve clinical outcomes.
• Topical treatment to the skin and affected mucous membranes helps reduce pain and complications.
• Multi-dermatomal zoster should alert the clinician to a patient with underlying immunosuppression.
need an explanation for this answer? contact us directly to get an explanation for this answer