History
A 29-year-old man presents with a nodule over his posterior trunk. He had recently moved into a flat with friends who had noticed the lesion and advised him to go to the GP. As far as the patient can remember he has had a mole on his back since childhood at the site of the nodule. He has Fitzpatrick skin type I and always burns in the sun, if not careful, and never tans. His family is also fair skinned. He is otherwise well and takes no medication.
Examination
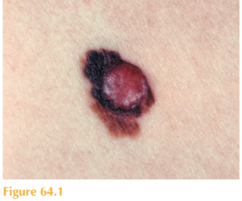
There is a reddish brown nodule arising from a deeply pigmented, irregular macule with variable colour (Fig. 64.1). Full skin examination reveals freckling over his face and shoulders and multiple acquired moles which looked benign.
Questions
• What is the likely diagnosis?
• What determines his prognosis?
• How should this patient be managed?
This young man has a nodular pigmented lesion on the posterior trunk that has changed in size, shape and colour. The clinical appearance of this lesion should immediately raise the possibility of a nodular malignant melanoma. Any patient concerned about a mole or skin lesion should have a full skin examination to check all their moles. A suspected melanoma should be excised for histological analysis with a 2-mm margin around it. The pathologist will report the thickness of the melanoma –the Breslow thickness (local invasion) in millimetres. This is the measurement between the granular cell layer to the deepest identifiable melanoma cell. The full skin check of a patient with a suspected malignant melanoma should also include examination of the lymph nodes.
The ‘gold standard’ treatment of melanomas is surgical. The extent of surgery depends on the thickness of the melanoma and its site. A small area of normal skin around the melanoma is also excised to ensure that all melanoma cells have been removed. This is termed a wide local excision (WLE). For lesions with a Breslow thickness of 1 m a 1-cm WLE is required; for lesions 1 mm a 2-cm WLE is advised. For these thicker melanomas a technique called a sentinel lymph node biopsy may be offered to patients
to exclude lymphatic spread. The sentinel lymph node biopsy can predict the presence of clinically non-detectable metastatic melanoma within regional lymph nodes through histopathology. The first node draining a lymphatic basin is termed the ‘sentinel node’.
If positive, a full basin clearance is offered and all the nodes are examined for further micro-metastases.
If the melanoma has spread to distant sites adjuvant therapies may be offered, but the prognosis is very poor. Distant metastases most commonly occur in lungs, liver, brain, bone and intestines.
Prognosis is determined by the staging classification: local disease T 1–4 a, b; disease in the regional lymph nodes N 1–3; and distant spread M 1a, b, c. The thinner the Breslow thickness, the better the prognosis. For those patients whose melanoma is 4 mm thick, 50 per cent will die within 5 years.
Following diagnosis, regular follow-up is essential to detect any recurrence. This includes local, lymphatic (lymph nodes) and blood borne (to distant sites). Examination of the scar site to exclude in-transit metastases, full skin examination, lymph node checks and palpation for organomegaly are required. A full systematic review should also be per-formed to exclude any distant spread. The periodicy and regularity of follow-up is also determined by the stage of the melanoma.
KEY POINTS
• Patients with a changing naevus should have a full skin examination.
• Breslow thickness measures the invasion depth of a melanoma in millimetres.
• Sentinel lymph node biopsy predicts clinically non-detectable metastatic disease.
need an explanation for this answer? contact us directly to get an explanation for this answer