History
A 39-year-old woman presents to the dermatology ‘two-week-wait’ clinic with a chang- ing pigmented lesion on her leg. Her partner reported that it had been changing over the last five months. She has type II skin and had moved to the United Kingdom from Australia 5 years previously. Whilst in Australia she had regular skin checks as her father had been diagnosed with malignant melanoma 6 years previously. She is otherwise well and takes no medication other than the oral contraceptive pill.
Examination
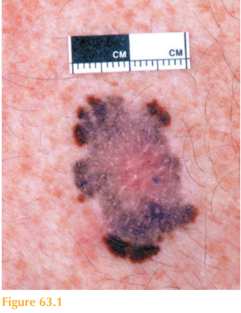
She has an asymmetrical, macular, variably pigmented lesion measuring 1.4 cm in dia-meter on her posterior calf (Fig. 63.1). With the dermatoscope the dermatologist notes a central whitish/blue area in the centre.
Questions
• What is the diagnosis?
• How would you determine the prognosis?
• What management would you organize?
This pigmented lesion looks highly abnormal as it is asymmetrical, has an irregular border and colour and therefore, clinically, is a malignant melanoma. This patient was brought up in Australia where ultraviolet light is intense; a change in the mole had been noted and she had a positive family history of malignant melanoma (MM).
Malignant melanoma is a malignant skin tumour of melanocytes. It is the most aggressive type of skin cancer. Its incidence has doubled in the past decade. Melanoma is amongst the commonest type of cancer in young adults. Approximately 30 per cent of melano-mas arise in a pre-existing naevus and the rest appear de novo. MM is more common in Fitzpatrick skin types I and II and has an increasing incidence closer to the equator. Then aetiology is complex, however. It is known that genetic predisposition and ultraviolet light exposure (particularly intermittent sun-burning episodes) are likely to play a role.
A pigmented lesion that demonstrates significant change should be excised to exclude melanoma. The A-B-C-D-E rule of melanoma is a useful tool for determining if a lesion is suspicious:
A – Asymmetrical shape
B – Border or Bleeding. The outline of a mole should be regular.
C – Colour. Benign naevi have a uniform colour. Those naevi with differing pigment should be evaluated carefully.
D – Diameter. Melanomas are usually 6mm in diameter.
E – Evolution: any change noted in a mole There are four main different variants of melanoma:
• Superficial spreading melanoma is the most common type and has a female prepon-derance. The lower leg is a common site. Clinically, the lesions are usually enlarging
brown/black macules with irregular margins and varying degrees of pigmentation. Somelesions may show signs of regression (areas of paleness/whiteness within).
• Nodular melanoma is more common in men and is most frequently reported on the posterior trunk. Clinically it appears as a pigmented papule or nodule that may ulcer-ate. During its horizontal phase of growth, the melanoma is normally flat, that is, superficial spreading melanoma. A nodular melanoma occurs as the vertical phase develops and the melano-ma becomes clinically thickened and raised.
• Acral lentiginous melanomas occur on the palmar plantar regions and subungal sites. They are the most common form of melanoma in Fitzpatrick skin types IV–VI. Acral melanomas may present as a pigmented macule or as a black area around the subungal skin and nail (Fig. 63.2). The diagnosis is frequently delayed due to the skin sites affected and patients’ lack of awareness, hence they often present late with a poor prognosis.
• Lentigo maligna melanoma is a melanoma that arises
within a lentigo maligna.
KEY POINTS
• Malignant melanoma (MM) is the most aggressive type of skin cancer.
• It is more common in Fitzpatrick skin types I and II.
• Variants include superficial spreading, nodular, acral and lentigo maligna melanomas.
need an explanation for this answer? contact us directly to get an explanation for this answer