History
A 7-week-old baby boy attends the paediatric dermatology clinic with his mother for follow-up of an extensive red patch. He was born at 38 weeks by elective caesarean sec-tion for transverse-lie, following an uneventful pregnancy. He has one sister. There is no family history of similar skin lesions. The red patch was noted at birth, and he was reviewed on a daily basis both by the dermatology department and by the neonatal team.
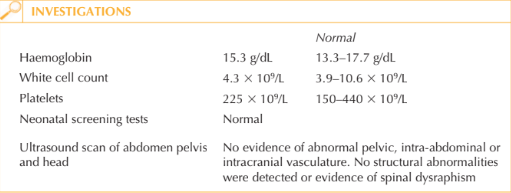
No other problems presented prior to discharge on day 5. In particular, his height and weight were both on the 50th centile, he was feeding well, passing urine and meconium.
A full blood count was performed prior to discharge and was normal, as was an ultra-sound scan of his abdomen, pelvis, spine and head. Since discharge he has continued to thrive, feeding from both breast and bottle. His mother has had contact with health visitors and dermatology specialist nurses and despite considerable initial anxiety is now calm and feels she is coping well.
Examination
His weight is now between the 50th and 75th centiles, with height and head circumfer-ence remaining on the 50th centile. He has an extensive, flat (macular), well-defined dusky red patch, which extends from the sole of his left foot along the posterolateral aspect of his leg to involve his entire left buttock and lumbosacral region (Fig. 53.1). He has a similar discrete patch on the left side of his upper abdomen, which extends posteriorly to the midline. Additionally he has a blue-grey macule over his right lum- bosacral area (a Mongolian blue spot). His observations are stable and examination of his cardiovascular, respiratory, abdominal systems and genitalia was normal. A detailed neurological examination revealed no concerns, his anterior fontanelle is level and he has a social smile. There is symmetry of all limbs.

Questions
• What are these patches?
• What complications can be associated with them?
• How should this child and his family be managed?
These lesions are capillary malformations or port wine stains. They represent congenital malformation of superficial dermal blood vessels as a result of abnormal morphogenesis. In the past, the nomenclature of these lesions has led to confusion and difficulty in dif-ferentiating vascular malformations from vascular proliferative lesions such as infantile haemangiomas. Capillary malformations are almost always present at birth (although not always detected because of neonatal plethora) and grow with the child; they remain present for life but may show tendency to colour change (either fading or more com- monly becoming a deeper purple). The surface can develop a cobblestone contour or nodularity in adulthood.
Thorough assessment of patients with capillary malformations for associated complica-tions is important. Capillary malformations can occur with other vascular malformations (venous, lymphatic, arterial or mixed). Ocular and/or central nervous system involvement occurs in approximately 10 per cent of patients with facial capillary malformations. In particular, involvement of the distribution of the ophthalmic division of the trigeminal nerve is associated with leptomeningeal involvement (Sturge–Weber syndrome), with risk of glaucoma, seizures, developmental defects, subdural haemorrhages and hemiple-gia. All patients with upper facial capillary malformations should have ophthalmological assessment (and magnetic resonance imaging of the brain if Sturge–Weber syndrome is suspected). Klippel–Trenaunay syndrome (angio-osteohypertrophy syndrome) is a triad of capillary malformation, congenital venous malformation and hypertrophy of the underly-ing tissues including muscle and bone. A capillary malformation overlying the spine may be associated with vascular malformations in the subjacent spinal meninges or occult spi-nal dysraphism. The coexistence of the capillary malformation and Mongolian blue spot in this case may be coincidental, however the literature suggests the risk of spinal structural or vascular anomalies is higher in the presence of another lumbosacral cutaneous anomaly.
Isolated capillary malformations are not associated with significant medical complica-tions; however, psychosocial disability secondary to disfigurement can be overwhelming. In the neonatal period such obvious and visible differences will inevitably be a source of anxiety for parents and it is crucial that the parents of this baby are offered sympathetic explanations, education and reassurance as well as the opportunity for them to discuss their concerns. They may benefit from peer support through patient support networks. This child will require long-term follow-up; if associated complications such as limb length discrepancy arise, he will benefit from the care of a multidisciplinary team including dermatology, orthopaedics, interventional radiology, plastic surgery, as well as occupational therapy, physiotherapy, and psychology. The treatment of choice for capil-lary malformations is pulsed-dye laser, which causes selective destruction of superficial abnormally dilated dermal bloods vessels, by inducing coagulation and rupture. The cos-metic outcome is variable, with larger lesions over limbs responding less well and tending to recur, compared to smaller lesions over the head and neck.
KEY POINTS
• Capillary malformations are congenital malformations of superficial dermal vessels, which are present at birth and grow with the child.
• They can be associated with other vascular malformations or structural anomalies.
• Isolated capillary malformations can be a source of significant psychosocial morbidity for new parents as well as for the affected individual.
need an explanation for this answer? contact us directly to get an explanation for this answer