History
A 63-year-old man presents to the dermatology out-patient clinic complaining of a non-healing ulcer on his right foot. He has had poorly controlled type 2 diabetes for 22 years. Four years ago his right big toe was amputated because of ulceration and infec-tion. Following that procedure his compliance with medication improved and he stopped smoking. He attends many different hospital appointments monthly and struggles with his weight because of chronic back pain and impaired vision. His medication includes metformin, glicazide, ramipril, amlodipine, aspirin and simvastatin.
Examination
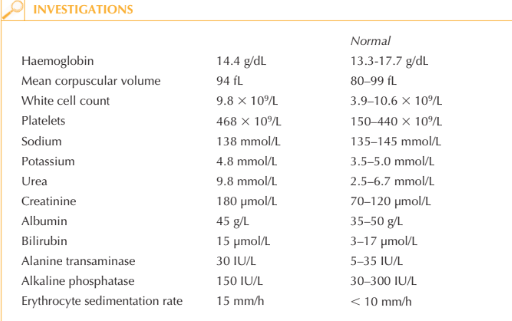
The patient is 1.85 m tall, weighs 104 kg and his blood pressure is 154/88 mmHg. He has a painless round ulcer overlying the right third metatarsal head, the base of which is covered with purulent slough. The ulcer is surrounded by callus formation with ery-thema and swelling extending medially and overlying the second metatarsal (Fig. 51.1).
There is no tissue crepitus but some scaliness of the surrounding plantar skin. There is onychodystrophy suggestive of onychomycosis affecting four of his nine toenails. He has reduced posterior tibial artery pulses bilaterally and absent dorsalis pedis pulse on the right. Ankle reflexes cannot be elicited. He is unable to sense 10-g monofilament pres-sure over the medial aspect of the distal third of his right foot; vibration, fine touch and
pin-prick sensation are also absent. Furthermore these modalities are reduced at both feet from approximately the ankle level.

Questions
• What factors described in the history and examination contributed to the ulcer?
• Which additional factors described above are risk factors for the development of foot ulceration?
• What additional tests would be performed at the bedside to assess diabetic complications?
• What is the management of this patient’s foot ulcer?
Foot ulcers affect 15–25 per cent of patients with diabetes. This patient’s peripheral neu-ropathy is likely to be the direct cause of an ulcer at this site. His elevated blood sugar, peripheral vascular disease and possible ulcer infection contribute to poor healing.
Callus formation often precedes ulceration and in this case reflects abnormal pressure distribution as a result of amputation and neuropathy. Diabetic foot ulcers occur typically over bony prominences of the feet, especially the big toe, or the plantar skin overlying the 1st or 2nd metatarsal heads. Complications of foot ulcers include soft tissue infection (cellulitis, fasciitis) and osteomyelitis. Lower extremity ulcers are a significant factor in amputations amongst diabetics.
Additional bedside tests would include urine dipstick – looking for proteinuria, in par-ticular – and lying and standing blood pressure, as the patient may be describing postural hypotension, a symptom of autonomic neuropathy. A scraping of the scaly areas can be taken to look for tinea pedis and the ulcer should be swabbed for bacterial culture.
Blood glucose monitoring may not be informative as it reflects only short-term control. It would, however, be important to check HbA1C level. The management of diabetic foot ulcers requires modification of factors that contribute to ulcer formation, for example, management of infection and glycaemic control. Standard therapy includes debridement, off-loading and protective dressings. Regular review and inspection of the ulcer is important. Ulcer prevention is one of the most important interventions medical professionals can provide for diabetic patients. Optimizing glycaemic control and patient education are crucial to ulcer prevention.
KEY POINTS
• Diabetic ulcers occur over bony prominences often within an area of callus formation.
• Poor glycaemic control, neuropathy and microvascular disease (with or without peripheral vascular disease) are important risk factors.
• Education and support from a multidisciplinary team are important.
• General foot care guidelines for patients with diabetes: daily washing of feet with lukewarm water and careful attention to drying; choice of appropriate footwear (always wear shoes and socks); daily inspection and palpation inside shoes to check for foreign objects or rough surfaces; seeking rapid professional attention for calluses, blisters, cuts, rash or ingrown toe-nails, etc.
need an explanation for this answer? contact us directly to get an explanation for this answer