History
A 34-year-old man presents to the dermatology clinic with multiple skin lesions on his limbs, which are asymptomatic and have increased in number over one year. He is other- wise well. On direct questioning he admits to shortness of breath whilst playing football.
Examination
He has multiple papules, nodules and annular lesions that are mainly scattered over his limbs (Fig. 47.1). These range in colour from tan/brown to purple. The skin overlying the lesions is slightly shiny and taut. On palpation of the lesions there is neither surface scale or textural change at the surface (epidermis normal), however there is marked induration (a firmness felt in the underlying tissue) indicating dermal pathology. The lesions are non-tender and skin temperature was normal. His temperature is 37 oC, blood pressure 124/87 mmHg, pulse 72 /min and oxygen saturation on air is 96%.

Questions
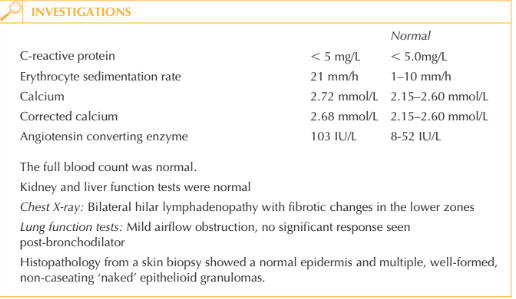
• What tests would you request to help confirm your diagnosis?
• What is your approach to this patient’s management?
This man has cutaneous and respiratory sarcoidosis. Skin lesions are classically asympto-matic and firm to touch. The involved skin is usually brown or slightly purplish in colour.
Papules, nodules, plaques and annular lesions are often seen. However, some patients may present with just a few flesh-coloured nodules on the face, or purple infiltrated nasal skin (lupus pernio). Some patients may have signs of erythema nodosum (tender nodules on the anterior shins), which results from an underlying panniculitis (inflammation of fat). Approximately 30 per cent of patients with sarcoidosis have cutaneous involvement.
Patients may have palpable lymphadenopathy or evidence of ‘bulky hilar’ on their chest X-ray. Formal lung function tests should be conducted in patients with respiratory symptoms and/or an abnormal chest X-ray. A skin biopsy from involved skin should be performed to help confirm the diagnosis. The histology classically demonstrates non-caseating ‘naked granulomas’ within the dermis. The aetiology of sarcoidosis is unknown but is hypothesized to be caused by a persistent antigen of mild virulence leading to chronic T-cell activation and granuloma formation.
Sarcoidosis is frequently managed by a multidisciplinary team, according to which organs are affected. If patients have solely cutaneous involvement, then lesions can be managed with superpotent topical or intra-lesional steroids, oral prednisolone, hydroxy-chloroquine or low-dose methotrexate.
This patient has significant respiratory as well as cutaneous involvement of his sarcoido-sis, therefore a systemic approach to his management is indicated. A short course of tapering oral prednisolone (20–40 mg daily) may be commenced initially before switch-ing to steroid-sparing low-dose methotrexate weekly for disease control.
KEY POINTS
• Cutaneous sarcoid can have a very heterogeneous appearance.
• Cutaneous lesions may signify underlying systemic disease, so always order a systems review.
• In multisystem disease the skin is often the most accessible organ for a histological diagnosis.
need an explanation for this answer? contact us directly to get an explanation for this answer