History
A 39-year-old patient presents to her GP with a rash of fairly sudden onset, which ini-tially affected her chest and arms and then spread to her back. She had noticed that the eruption started as small red spots that were dry and scaly, which then spread out in a ring-shape. She was worried she might have caught ring-worm in the school where she works. However, it seemed to start after her recent holiday in Spain. The rash is asymp-tomatic. She has no previous history of skin problems, and is otherwise well.
Examination
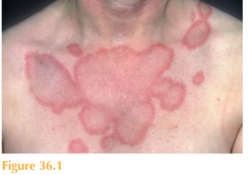
There is an erythematous eruption predominantly affecting her face, neck, trunk and proximal limbs. The lesions are annular in appearance, sharply defined with an overly-ing surface scale. The lesions display central regression and coalesce to give a polycyclic appearance (Fig. 36.1). Her scalp nails and mucosae are normal.
Questions
• What is the cutaneous diagnosis?
• What systemic manifestations may beassociated?
• How should this patient be managed?
This patient presented with the classic skin eruption of subacute cutaneous lupus ery-thematosus (SCLE). The rash appears fairly suddenly, especially over sun-exposed sites, and is symmetrical and scaly. There are characteristically bright red, annular, well-demarcated lesions with central regression. Overlying the erythema there is an almost psorisiform scale. The eruption mainly affects the upper trunk (shoulders and ‘V’ of the chest) and dorsi of the hands (sun-exposed sites). SCLE occurs in young and middle-aged patients and is more common in females. It is usually a very persistent eruption lasting many months.
Approximately 50 per cent of patients will also meet a few of the criteria for systemic lupus erythematosus (SLE) as defined by the American Rheumatism Association (see also Table 35.1). These mainly include photosensitivity, arthralgia, serositis and serologic abnormalities. The serious organ involvement of SLE is uncommon, although renal and CNS involvement can rarely occur and thus all SCLE patients should be investigated for systemic disease.
Virtually all patients with SCLE have circulating anti-Ro (SS-A) and 30–50 per cent will have anti-La antibodies. Pregnant women with Ro (SS-A) positive SCLE may give birth to babies with neonatal lupus due to placental transfer. The rash is morphologically similar to SCLE, but is transient. More seriously, congenital heart block can occur. The heart block is usually permanent requiring a pacemaker and all women of child-bearing age should be counselled accordingly. Coexistent Sjörgren’s syndrome with SCLE has been reported.
A comprehensive drug history is essential in patients with SCLE, as the disease can be triggered by certain medications including naproxen, nifedipine, verapamil, diltiazem and terbinafine.
Cutaneous disease is most often the commonest concern of patients. Sun avoidance and photoprotection are essential in all patients. Some patients do respond to potent topi-cal corticosteroids, but many require systemic therapy to control the cutaneous disease, including thalidomide and hydroxychloroquine. A small proportion of patients may go on to develop SLE.
KEY POINTS
• The rash of subacute cutaneous lupus erythematosus (SCLE) characteristically displays erythematous annular lesions with central regression.
• 50 per cent of patients with SCLE will also have a few of the criteria of SLE.
• Virtually all patients with SCLE have circulating anti-Ro (SS-A) antibodies.
need an explanation for this answer? contact us directly to get an explanation for this answer