History
A 67-year-old woman presents to the accident and emergency department with a 6-day history of severe, painful and progressive blistering. She had attended her GP eight weeks earlier with a worsening ‘burning itchy’ eruption. She had been diagnosed with urticaria and been started on a regular antihistamine with no benefit. Two weeks ago she had attended her dental practitioner with painful oral erosions, and is awaiting specialist review. Her past medical history includes a cholecystectomy and borderline abnormal thyroid function tests, for which she is on no therapy currently. She is an ex-smoker. There are no other remarkable features in her history.
Examination
The patient is clearly uncomfortable at rest and it is painful for her to move during the examination. She has two small ( 5 mm) healing erosions on her right buccal mucosa and a fresh tense blister (~7 mm) on her hard palate. The rest of her oral examination is normal. She has a symmetrical erythematous urti-cated eruption over the lateral aspects of her trunk, her submammary area, medial upper arms, and thighs and central back. Within these erythematous lesions there are multiple tense fluid-filled vesicles ( 5 mm) and bullae ( 5 mm) (Fig. 28.1). Her geni-tal mucosa is normal. The remainder of her physical examination is normal.

Questions
• In addition to establishing a diagnosis, what are the immediate priorities in the manage-ment of this patient?
• What are the likely diagnosis and the possible differential diagnoses?
• What is the long-term prognosis?
This is clearly a widespread, evolving and aggressive, blistering eruption. In addition to establishing a diagnosis and ruling out any underlying medical disorders, the priorities for this patient are pain relief and prevention of infection. Pain relief would include simple measures such as reducing friction to eroded areas of the skin (with easy-release dressings and/or greasy emollients) and minimizing activity, as well as pharmacological pain relief. Preventing infection can be challenging: barrier nursing and use of topical antiseptics such as potassium permanganate, triclosan and chlorhexidine, particularly when washing, are frequently advocated.
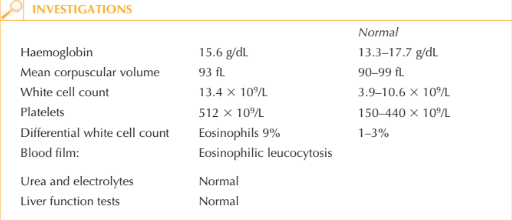
The age of the patient, her history and presentation, and eosinophilia are highly sug-gestive of a diagnosis of bullous pemphigoid. Other autoimmune bullous diseases could be considered in the differential diagnosis, in particular: inflammatory epidermolysis bullosa acquisita (a mucous membrane pemphigoid, which often has a more insidious onset with more mucosal involvement than skin); erythema multiforme major (usually more haemorrhagic mucosal involvement and targetoid lesions); and bullous vasculitis (usually purpuric skin lesions in association with blistering, especially of the lower extremities). Occasionally bullous pemphigoid can be associated with underlying conditions such as inflammatory bowel disease or occult malignancy or be provoked by medication (e.g. furosemide, ACE inhibitors, and recently anti-TNF monoclonal antibody therapy).
Bullous pemphigoid is characterized by circulating and tissue-bound pathogenic anti-cutaneous basement membrane zone antibodies. These can be detected by immunofluorescence studies (on skin and serum). Figure 28.2 demonstrates posi-tive green fluorescence of tissue-bound antibodies along the cutaneous basement membrane. Immunosuppression with sys-temic corticosteroids and steroid-sparing agents is the cornerstone of treatment; although for patients with milder or more localized disease superpotent topical cor-ticosteroids alone may be sufficient to achieve disease control. Remission over a period of years is expected; however, prog-nosis is adversely affected in the elderly by their frequent co-morbidities.
KEY POINTS
• Bullous pemphigoid frequently affects elderly individuals, presenting as painful tense bullae on a pruritic urticated base. Mucosal involvement is not usually a major feature.
• As well as the necessary investigations to confirm the diagnosis, co-morbidities and occult underlying diseases should be sought prior to initiation of immunosuppressive therapy.
• The natural history is for bullous pemphigoid to remit over years, but the adverse effects of immunosuppressive treatment on the elderly can be significant.
need an explanation for this answer? contact us directly to get an explanation for this answer