History
A 62-year-old man presents to the accident and emergency department with a 2-day history of an asymptomatic skin eruption appearing mainly on his trunk and limbs. It seems to have started after visiting his local swimming pool and he had wondered if the chlorine in the water may have triggered the skin rash. He is otherwise fit and well but has recently had a sore throat and temperature but no cough. He has no previous history of skin problems. He is referred to the on-call dermatology team.
Examination
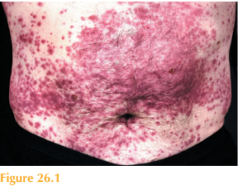
There is a widespread eruption mainly on the lower limbs and trunk but also to a lesser extent on his arms. The morphology of the rash is purple and non-blanching; lesions are starting to coalesce and are mainly macular but some are papular (Fig. 26.1). His tonsils are erythematous with some surface exudate and he has tender cervical lymphadenopathy. His temperature is 38.7 °C.
Questions
• What is the likely cause of the skin eruption?
• What pathological process would be seen on the skin histopathology?
• What is the differential diagnosis of this skin rash?
Non-blanching skin eruptions usually indicate bleeding into the skin, blockage of cutane- ous blood vessels or reduced blood flow (viscosity/stasis). The underlying cause may be benign such as pressure on the skin, or serious such as bacterial meningitis. Small pin-point areas of bleeding into the skin, so-called ‘petechiae’, can occur due to leakage from small cutaneous capillaries (capillaritis), pressure on the skin (from tight bandages/compression stockings) or vascular damage due to infections. Larger areas of bleeding into the skin (ecchymoses) can occur on the limbs of elderly patients following minor trauma, as their skin is thin and fragile. Macular areas of purple non-blanching skin are usually the result of red cell leakage or bleeding (low platelet count). Palpable purpura by contrast is usually associated with an acute inflammatory process such as vasculitis. Acute and severe vascular damage may result in skin necrosis.
This patient had acute vasculitis (leucocytoclastic vasculitis), which is inflammation of the blood vessels. This inflammation leads to leakage of red cells and ultimately block-age of skin blood vessels. Skin biopsy is extremely helpful in confirming the clinical suspicion of vasculitis. Histology from affected skin shows tissue swelling, perivascular inflammation and fibrin blocking cutaneous blood vessels. Neutrophils around the ves-sels are frequently killed (leucocytoclasis) and remnants of them (‘nuclear dust’) are seen scattered in the dermis.
The throat swab from this patient confirmed a streptococcal infection, which is the likely underlying cause of his vasculitis. He was treated with oral penicillin V and potent topi-cal steroids. The differential diagnosis of a vasculitic rash includes bacterial meningitis, Streptococcus, hepatitis C/B, autoimmune diseases (lupus, polyarteritis nodosa, rheumatoid), drug reac-tion and malignancy. Investigations of cutaneous vasculitis might include the following: skin biopsy, urine dipstick (for blood/casts), full blood count, erythrocyte sedimentation rate, renal/liver function, streptococcal serology (ASOT), hepatitis serology, antinuclear antibodies (ANA), extractable nuclear antibodies (ENA), antineutrophil cytoplasmic antibodies (ANCA), rheumatoid factor, coagulation screen, antiphospholipid antibodies, blood pressure, and chest X-ray.
KEY POINTS
• Acute-onset non-blanching purple skin eruptions can indicate a serious underlying cause.
• Skin biopsy can help to distinguish between true vasculitis and simple blood vessel leakage.
• A vasculitis screen may help to elucidate the underlying cause.
need an explanation for this answer? contact us directly to get an explanation for this answer