History
A 41-year-old woman presents to the on-call medical team with a fever and mild malaise. She complains of a sore rash with pustules appearing on her trunk and limbs over the past 24 hours. She was previously fit and well with no history of previous skin problems. There is no family history of note. She had been taking a herbal preparation over the past few months but this had stopped 3 weeks ago. She is currently taking a course of penicillin prescribed by her GP 3 days earlier.
Examination
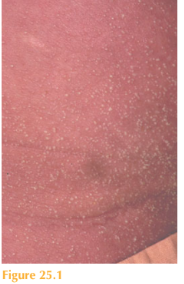
The patient has a temperature and looks unwell. She has a widespread erythema over her trunk and limbs that is studded with multiple, small monomorphic pustules (Fig. 25.1). There is a predilection for the flexural areas. Nikolsky’s sign is negative. Mucous membranes, nails and scalp are normal. Her temperature is 38.4 °C.
Questions
• What is the cutaneous diagnosis?
• What is the likely cause?
• How would you manage this patient?
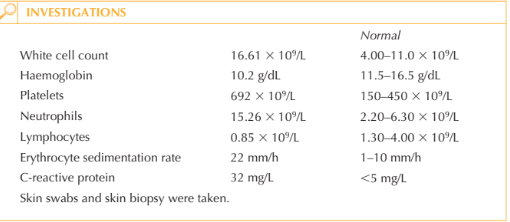
This patient presented with a very dramatic tender skin eruption called AGEP (acute gen-eralized exanthematous pustulosis). This is a pustular drug eruption, most likely caused in this case by penicillin. AGEP is characterized by multiple pin-point pustules which are very monomorphic in nature and appear in sheets on an erythematous background. There is often accentuation in the flexural areas such as axillae and groin. Swabs are negative for organisms as the pustules are sterile. In contrast infected cutaneous pustules tend to be at different stages of evolution varying in size and shape, the erythema tends to be localized around each pustule rather than diffuse; lesions may be crusted. The differential diagnosis includes acute pustular psoriasis. Some patients may have a past history of psoriasis (usually the chronic plaque form) in which the skin suddenly becomes unstable (this can be triggered by oral prednisolone) and develops multiple sterile pustules within the psoriatic plaques. Pustules are usually prominent around the periphery of the areas of erythema rather than as sheets of pustules throughout. Rarely, it may be difficult to differentiate between AGEP and pustular psoriasis, as some patients’ first presentation of psoriasis may be with the acute pustular form. Pateints with AGEP frequently have a fever and mild to moderate malaise. Blood tests usu-ally show a neutrophilia and a mildly raised CRP. Patients may therefore be misdiagnosed as having a skin infection due to staphylococcal bacteria. Histology from the skin biopsy shows subcorneal collections of neutrophils, which is supportive of the diagnosis of AGEP. In psoriasis there is usually an associated thickening of the epidermal skin layer – so-called acanthosis – which is absent in AGEP. The drug implicated in AGEP should be stopped immediately if at all possible. Pustules usually resolve over 1–2 weeks. To speed the cutaneous recovery, systemic corticosteroids should be given. Topical treatment with 50:50 white soft paraffin with liquid paraffin should be applied to the skin every 2 hours in the acute phase. Secondary infection by Staphylococcus bacteria to eroded areas can occur before the skin heals. In the mean-time patients can loose heat and fluids through their impaired skin barrier causing high insensible fluid losses.
KEY POINTS
• AGEP is an acute-onset drug eruption characterized by sheets of monomorphic pustules on red skin.
• The pustules in AGEP are sterile and represent a toxic drug reaction and not a skin infection.
• The culprit drug should be stopped and systemic/topical steroids used to treat the patient.
need an explanation for this answer? contact us directly to get an explanation for this answer