History
A 51-year-old man is referred for an urgent opinion with an 8-week history of intermittent swellings affecting his hands, feet, face and genitalia. He also describes intermittent abdomi-nal bloating and pain. Over the last three weeks he had attended the accident and emergency department on two occasions. The first time, when he presented with lip and tongue swelling but without shortness of breath, he was treated with antihistamines and intravenous hydro-cortisone, but did not require adrenaline or intubation. On the second occasion, with acute and severe abdominal pain associated with vomiting, he was admitted for 24 hours under the surgical team for investigation of an acute abdomen, before his symptoms spontaneously resolved. He does not describe any associated urticaria but does complain of recent-onset night sweats, weight loss and low energy levels. He is unaware of provoking factors and feels there is no pattern to the swellings as they can occur at any time including overnight. He has no previous history of atopy and is on no medi cation (he denies taking any over-the-counter prep arations such as non-steroidal anti-inflammatory drugs). He has no family history of swellings or skin rashes. He is a non-smoker and works as a truck driver.
Examination
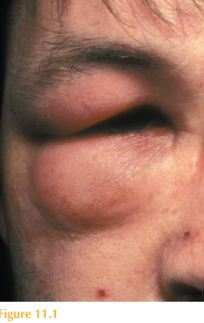
His skin is normal except for the presence of uni-lateral left-sided peri-orbital soft tissue swelling (Fig. 11.1). He has smooth, non-tender bilateral axillary and left-sided inguinal lymphadenopathy. The remainder of his examination is normal.
Questions
• What are these intermittent swellings?
• What are the possible underlying diagnoses?
• How would you investigate further?
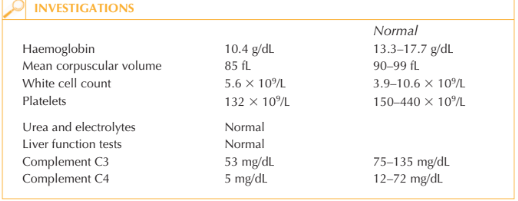
The skin swellings are angioedema. Unusually in this case angioedema is occurring in the absence of urticaria. Immunoglobulin E (IgE)-mediated allergic angioedema (provoked by food, drugs, insect bites or latex) or angioedema provoked by physical stimuli (such as sun, heat or cold) is mediated by local release of histamine and is frequently associated with hives or urticaria. The striking other clinical features in this case include the night sweats, weight loss and lymphadenopathy. He has anaemia and thrombocytopenia. The low complement levels should trigger testing of C-1 esterase inhibitor (C1-INH) levels (suggesting acquired C1-esterase inhibitor deficiency). This patient needs thorough haematological assessment looking for an underlying lymphoproliferative disorder. Further investigations include tests for serum lactate dehydrogenase and 2-microglobulin, immunoglobulins and protein electro-phoresis, CT of the chest, abdomen and pelvis as well as lymph node and bone marrow biopsy. When confronted with angioedema in the absence of urticaria it is important to con-sider diseases mediated by bradykinin such as C1-INH deficiency (which can be genetic or acquired) or induced by angiotensin converting enzyme (ACE) inhibitors. Hereditary angioedema is autosomal dominantly inherited, and although there is a high incidence of de-novo mutations (25 per cent), it usually presents peri-puberty or following sur-gery/trauma, making it a less likely diagnosis in this case. Acquired angioedema can be associated with underlying connective tissue disease (systemic lupus erythmatosus, lupus anticoagulant) or lymphoproliferative (particularly B-cell lymphoma) disorders. Common to all of these disorders are symptoms of angioedema, in the absence of urticaria, which can include laryngeal oedema or tongue and/or pharyngeal oedema of sufficient severity as to cause airway obstruction and, potentially, asphyxia. These bradykinin-dependent disorders can also include gastrointestinal symptoms reminiscent of an acute abdomen with severe pain, nausea, vomiting, or diarrhoea due to oedema of the bowel wall. Hypotension is frequently a feature. The management of acquired angioedema includes the use of androgens (such as dana-zol or stanozolol) and antifibrinolytics (such as tranexamic acid) as prophylaxis. The emphasis however is on diagnosis and treatment of the underlying disease. For heredi-tary angioedema, C1-INH concentrate (extracted from human plasma and freeze dried) is available for intravenous administration.
KEY POINTS
• Angioedema in the absence of urticaria is unusual and points towards a bradykinin-mediated mechanism, most commonly C1–INH deficiency, either hereditary or acquired.
• Symptoms may include angioedema of the face, extremities and genitalia, abdominal pain and bloating, hypotension and potentially laryngeal oedema leading to asphyxiation.
• Underlying autoimmune connective tissue disease or B-cell lymphoproliferative disorders may underlie acquired angioedema.
need an explanation for this answer? contact us directly to get an explanation for this answer