History
A 16-month-old boy presents to the dermatology clinic. His mother has noticed a gradual accumulation of ‘brown spots’ on his skin. These lesions were not present at birth and the majority appeared as a crop over a 4-month period around his first birthday. She feels it is possible that he will continue to acquire new lesions. He had one on his right forearm which has resolved. She has noticed that some of the lesions appear to ‘blister’ or become raised after a bath. He is otherwise well; he is thriving and enjoys a full diet. He has no gastrointestinal symptoms or wheeze. There is no family history of similar skin lesions. The rest of the family is entirely well.
Examination
His height and weight are on the 75th and 91st centiles for his age, respectively. He is coop- erative and follows directions. He has diffuse, scattered, monomorphic, small oval-round reddish-brown macules concentrated predominantly over his anterior and posterior trunk, but also extending to his neck and with a few scattered lesions on his limbs. There are more than 40 of these lesions. One lesion just below his xiphisternum, when rubbed, became tran- siently erythematous and swollen (urticaria), a positive Darier’s sign (Fig. 10.1). Examination of his cardiorespiratory system and abdomen is normal. He has no lymphadenopathy.

Questions
• What are these lesions?
• Would you perform any further inves-tigations?
• What is their management?
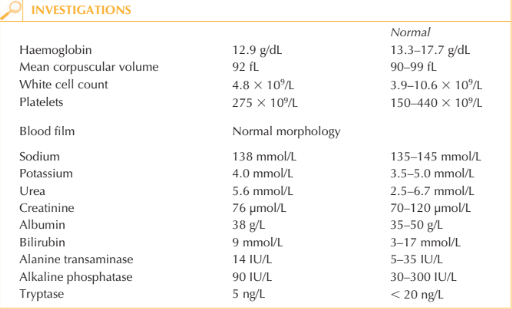
These lesions represent multiple mastocytomas and the eruption is referred to as urti-caria pigmentosa. Darier’s sign describes the development of a wheal and surrounding erythema in a lesion after rubbing (physical degranulation of histamine from mast cells). Mastocytosis is the abnormal accumulation of mast cells within the skin and rarely other organs (liver, spleen or lymph nodes). The differential diagnosis would include lentigines or melanocytic naevi (if Darier’s sign negative) or xanthogranuloma, histiocytosis X or generalized eruptive histiocytoma (if the lesions were raised or indurated). All forms of mastocytosis in children have a good prognosis and systemic involvement is rare. The majority of cases resolve spontaneously. In adults, however, systemic involve-ment may be aggressive or even represent a mast cell leukaemia. Symptoms of systemic involvement or of acute degranulation of widespread cutaneous disease include flushing, diarrhoea, nausea/vomiting, abdominal cramps and wheeze. Adults may also complain of syncope, angina, headaches and bone pain. Although this young patient has no symptoms of systemic disease, basic investigations would be justified including particularly full blood count, serum tryptase and liver func-tion tests. A skin biopsy can be performed if there is diagnostic doubt. Mast cell infiltrates can be difficult to identify by routine haematoxylin & eosin staining, and special stains such as Giemsa or toluidine blue, which demonstrate metaochromatic staining of mast cells, are required. For patients with rapidly progressive disease and abnormalities of the above investigations, further testing such as bone marrow aspirate and biopsy under the supervision of the haematology department may be indicated. Demonstration of activat-ing mutations of the c-kit proto-oncogene would help tailor therapy in aggressive or leukaemic disease (e.g. imatinib). As the skin lesions are likely to resolve spontaneously by the boy’s 10th birthday, no treatment is indicated. For patients with skin symptoms antihistamines (H1-blocker) may be helpful. Moderate sunlight exposure can hasten the resolution of diffuse lesions and psoralen–UVA can be offered to adults/older children. Patients with numerous lesions or diffuse disease should avoid mast cell degranulating agents such as non-steroidal anti-inflammatory drugs, opiates, alcohol, caffeine, radiological contrast media and abrupt physical degranulation such as a hot bath or other acute temperature change, vigorous rubbing (e.g. after a bath or by tight clothing). Exposure to degranulating agents or to allergens (such as hymenoptera stings) can potentially provoke anaphylaxis.
KEY POINTS
• Urticaria pigmentosa is characterized by mast cell proliferation and accumulation within the skin.
• When a urticaria pigmentosa or mastocytoma lesion is stroked, it typically urticates, becoming pruritic, oedematous and erythematous. This change is referred to as Darier’s sign.
• Most patients with urticaria pigmentosa exhibit onset before age 2 years. The disease is associated with an excellent prognosis, often with resolution by puberty. The number of lesions diminishes by approximately 10 per cent a year.
need an explanation for this answer? contact us directly to get an explanation for this answer