History
A 26-year-old woman attends the dermatology clinic complaining of a 4-month history of an itchy eruption. She describes the eruption as ‘cloud-like’. She previously suffered from eczema as a child but this rash is different. She tells you that although the eruption waxes and wanes, with individual lesions lasting 8 to 12 hours, she is rarely clear of lesions for more than half a day. Sometimes she goes to bed with the eruption and wakes clear, but the opposite can also occur. She has never experienced angioedema. She tells you it is often worse peri menstrually. You question her about possible precipitants; she tells you that the eruption is worse with exercise or a hot bath, but does not appear to be aggravated by pres- sure or cold. The eruption is partially attenuated by cetirizine 10 mg daily, which she is tak-ing for her hayfever. Her only other medication is occasional ibuprofen for dysmenorrhoea. There is no family history of skin lesions. Both of her parents are well, although her mother has a diagnosis of osteoporosis and is on thyroxine replacement. On close ques-tioning she admits that although circumstances at work are stable and have not changed for a longtime she is experiencing difficulty coping and frequently cries at work.
Examination
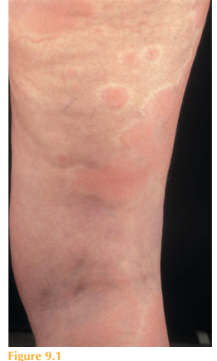
On examination there are several scattered lesions over her trunk, limbs and face. They are composed of well-defined erythematous oedematous plaques surrounded by a pale ‘flare’ (Fig. 9.1). The lesions vary in size and shape but not in morphology. You are unable to elicit dermographism. The lesion that you ringed initially had disappeared by the time she presented to photography 2 hours later, with new lesions developing over adjacent skin.
Following their resolution the lesions leave no persistent skin change. Although the eruption is pruritic there is no evidence of lichenification or excoriations. Her blood pressure is 105/68 mmHg and pulse rate 102 beats/min. Examination of her cardiorespiratory system is otherwise normal. Her abdomen is soft and non-tender. You notice a degree of bilateral upper eyelid lag. She has a smoothly enlarged goitre and stretching her hands out she has a fine tremor.
Exaination of the remainder of the neurologi- cal system is normal. Urinalysis was negative for blood, white cells and glucose. You ask the patient to put on her coat and walk briskly up and down the corridor outside. After five minutes she returns with a marked aggravation of her eruption, which is now widespread and generalized over her trunk and proximal limbs. You draw around a well-defined skin lesion and request some further investigations.
Questions
• What is this eruption?
• What factors in the history and on examination might be contributing to the eruption?
• How would you investigate this patient?
• What is the management?
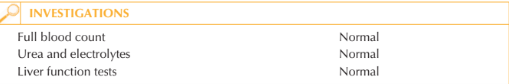
This patient is suffering from urticaria, which is characterized by wheals or ‘hives’ that represent areas of cutaneous mast cell degranulation, releasing histamine and other mediators, followed by transient oedema and erythema. When urticaria persists for more than 6 weeks it is classified as chronic urticaria. It represents a tissue reaction pattern and can be precipitated by a variety of stimuli or triggers. Many skin eruptions are known which may present with ‘urticated’ lesions that are not transient. There may be more than one precipitant of urticaria in any one affected individual. Although there is an element of physical provocation, which you have demonstrated by exercising the patient, the eruption can be present on waking and therefore there is more to this than cholinergic urticaria. The patient is atopic, a factor reported to be associ-ated with urticaria. She has made an interesting observation that her urticaria is worse peri-menstrually; the phenomenon of progesterone-provoked urticaria is described. It is more likely, however, that the exacerbation is due to her use of a non-steroidal anti-inflammatory drug (ibuprofen). Importantly, she has clinical features of thyrotoxicosis –chronic urticaria is associated with a number of autoimmune diseases, particularly autoimmune thyroid disease (Graves’ disease), systemic lupus erythmatosus (SLE) and cryoglobulinaemia. Urticarial vasculitis is an important differential diagnosis of chronic urticaria. Typically the lesions of urticarial vasculitis are associated with a burning pain and persist for more than 24 hours. They may leave post-inflammatory hyperpigmentation or ecchymoses on resolution and can be diagnosed by the demonstration of a leucocytoclastic vasculitis on biopsy of affected skin. Where urticarial vasculitis is suspected a work-up for potential systemic vasculitis is important. The initial investigation of this patient would include complete blood cell count, eryth-rocyte sedimentation rate, thyroid function tests, antithyroid antibodies (antithyroid microsomal and peroxidase antibodies), basophil histamine release assay. Other tests which might be considered: skin biopsy, antinuclear antibodies (ANA), C3, C4 (if features of urticarial vasculitis or associated angioedema suggesting acquired C1 esterase defi-ciency secondary to SLE), cryoglobulins and cryoprecipitans (if history of cold-induced urticaria). It is clear that this patient has symptomatic thyrotoxicosis, so its management and control may significantly improve or even resolve her urticaria. In the short term pro-pranolol may be indicated until carbimazole achieves a euthyroid state. For any persisting urticaria non-sedating antihistamines (anti-H1) are the mainstay of treatment. Response to different antihistamines can vary so it may be worthwhile trialling different agents, and in some cases doses higher than those required in allergic rhinoconjunctivitis may be needed. The addition of anti-H2 antihistamine such as ranitidine or cimetidine may provide some additional blockade of histamine receptors and can be beneficial, as can the addition of a leukotriene receptor antagonist such as montelukast. In general these agents are well tolerated. For patients with evidence of autoimmune association and trouble-some persistent urticaria, immunosuppressive therapy with agents such as ciclosporin or methotrexate may be required.
KEY POINTS
• Urticaria is a cutaneous reaction pattern characterized by the degranulation of mast cells and transient wheals.
• There are a number of potential precipitants, exacerbating factors and underlying causes of chronic urticaria.
• The mainstay of therapy is to correct any underlying medical disorders and the use of non-sedating anti-H1 antihistamines.
need an explanation for this answer? contact us directly to get an explanation for this answer