History
A 67-year-old woman presents to the vascular surgeons with varicose veins. She had a history of venous ulceration in the past, which has now healed and she is being consid-ered for bilateral varicose vein surgery. At the consultation she complained of a 3-month history of skin itching and redness, particularly on the right lower leg, and was noted to have unilateral erythema and was referred to dermatology for an opinion.
Examination
This patient has obvious dilated and tortuous veins on both lower legs. Confluent back-ground dull erythema is seen on the right lower leg, with small inflammatory superficial erythematous erosions and excoriations (Fig. 6.1). Palpation revealed warm, dry, rough skin at the affected site.

Questions
• What is the diagnosis?
• What treatment would you recommend for her right leg prior to vein surgery?
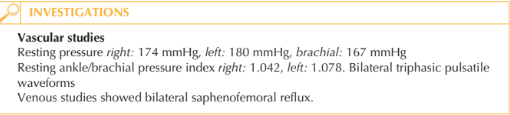
• Is this patient suitable for compression hosiery based on the vascular studies?
This patient has chronic cutaneous changes seen on the right lower leg consistent with the diagnosis of varicose eczema. This common cutaneous eruption usually has an insidi-ous onset over many weeks to months in patients with a background of venous incompe-tence. The affected skin is pruritic and dry with marked erythema which may be variable in intensity depending on its chronicity. In the context of venous insufficiency, pitting oedema may develop owing to poor venous return leaving the skin tight and oedema-tous. This results in reduced blood flow to the skin, leading to active dusky erythema and resultant erosions or even ulceration. Varicose eczema can be readily distinguished from cellulitis affecting the lower leg. Varicose eczema usually develops slowly, is frequently bilateral, pruritus is marked, the skin surface is rough and dry, and there are associated varicose veins. Frequently there is a background brown discolouration of the affected skin area due to haemosiderin deposi-tion. Haemosiderin pigment is derived from haemoglobin, which is left behind in the skin when red blood cells extravasate into the tissue. Management of the skin requires a combination of topical therapy and if possible com-pression. The leg should be washed with aqueous cream or an antiseptic emollient such as Dermol 500®. A moderately potent topical steroid should be applied to the eczematous areas and a rich bland emollient. Compression hosiery or two to four layer bandaging is essential to ‘squeeze’ the fluid out of the legs and allow skin healing. If the ankle/brachial pressure index (APBI) is above 0.8 then the arteries are sufficiently patent to permit compression without compromising the arterial blood supply to the lower extremities.
KEY POINTS
• Varicose eczema can be distinguished from cellulitis by slow onset, pruritus and surface xerosis.
• Management of the eczema will not succeed without addressing the underlying oedema.
• Potent topical steroids should be applied to the active eczema areas plus emollients and compression.
need an explanation for this answer? contact us directly to get an explanation for this answer