History
A 5-year-old girl who is well known to your practice attends with her mother. She has been troubled by worsening pruritus over the last six weeks. She has missed more than ten days of school in the last month. Her mother reports that she wakes frequently at night and is lethar-gic and moody during the day. Her bed sheets are covered in flecks of blood in the morning. The girl is known to be allergic to egg, fish and peanut, and has begun to develop the symptoms of seasonal allergic rhinoconjunctivitis within the last couple of months. She has a positive family history of atopy, both parents are allergic to animals and her older brother has asthma. Her younger brother has been sent home from nursery with impetigo recently. Her treatments include an emollient as soap and leave-on preparation and various strengths of topical steroids ranging from very mild to moderately potent depending on site and eczema severity. On questioning, however, mother reports that her daughter’s skin is so sore that she is refusing to bathe or apply her topical treatment.
Examination
A full examination reveals a fractious child; she is unable to stop scratching her skin once undressed. She is slim, with her height at the 25th centile and weight at the 4th centile for her age. She has widespread, mildly tender, shotty lymphad-enopathy (cervical, axillary and groin). Her skin is generally mildly erythrodermic and extensively excoriated, particularly her limbs (Fig. 2.1), neck and lower back. The excoriations are covered with haemorrhagic crust and yellowish exudates.

Questions
• What is the primary diagnosis?
• What secondary complications are exacerbating her pruritus?
• How would you manage this patient?
The primary diagnosis is atopic eczema associated with a positive family history of atopy as well as manifestations of IgE-mediated (immediate-type) hypersensitivity (food allergy and allergic rhinoconjunctivitis). This is clearly a moderate to severe flare of her eczema.
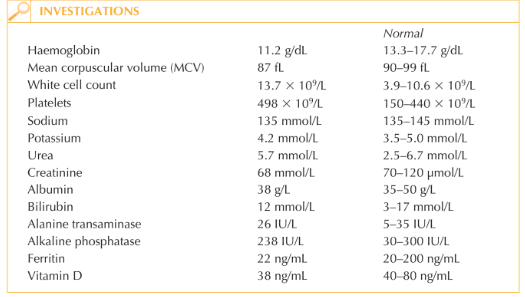
The severity of eczema can be ‘scored’ by various validated subjective (e.g. CDLQI – chil-dren’s dermatology life quality index) and objective scoring systems. Crudely, however, the impact on sleep and school attendance as well as the clinical severity of her eczema demonstrated in the photograph denotes severe eczema with significant functional disruption. There may be several factors contributing to the current flare. It is likely that there is an element of secondary infection with Staphylococcus aureus or impetiginization of this child’s eczema. The extensive yellow crusting of her excoriations, her tender lymphad-enopathy, and the fact that her brother has impetigo, suggest colonization of the patient and potentially other family members. Difficulty in adhering to a bathing regime is likely to contribute. Other potential factors which worsen pruritus include iron deficiency. She is also vitamin D deficient, presumably due to her dietary restriction (egg and fish are the main dietary sources of vitamin D). It is important to gain control of this child’s eczema rapidly. Swabs should be taken for microbiology culture and sensitivity testing both from the patient and her immediate family members. As there appear to be at least two members of the family affected by Staphylococcus aureus it would be worthwhile considering Staphylococcus eradication protocol for the entire family (i.e. antiseptic washes and antibacterial nasal ointment). The patient might benefit from a 5–10-day course of antibiotic with good Staphylococcus aureus coverage (first line: flucloxacillin; second line: erythromycin or co-amoxiclav). The extensive use of a moderately potent topical corticosteroid ointment for 2–4 weeks may be required before weaning back to weak preparations or calcineurin inhibitors as maintenance therapy.
KEY POINTS
• Atopic eczema is by definition eczema associated with a personal and/or family history of atopy.
• Staphylococcus aureus may cause severe flare of eczema.
• Management of such a flare includes Staphylococcus aureus eradication as well as appropriate treatment of the eczema.
need an explanation for this answer? contact us directly to get an explanation for this answer