A SWOLLEN SHOULDER
History
Naomi is a 13-year-old girl who presents to the A&E department of her local hospital for the third time in 8 weeks. On the first occasion she had slipped from her horse whilst mounting and sustained some minor bruising mainly to the right arm, hip and leg. There was no evidence of any serious bone injury. Over the course of the next 2 weeks she developed worsening pain and immobility in her right shoulder. Examination from that visit was recorded as showing a decreased range of movement but little else. Her symptoms were thought to be due to either a ‘frozen shoulder’ or to be functional, and she was prescribed ibuprofen for pain and referred for routine physiotherapy. The physiotherapists have sent her back with increasing pain and now swelling.
Examination
Naomi is clearly in pain and is reluctant to move her right shoulder. There is a generalized, smooth, warm, firm swelling of the right shoulder with a decreased range of movement in all directions. There are some distended visible veins and the overlying skin is shiny but not red. The remainder of the examination is normal.
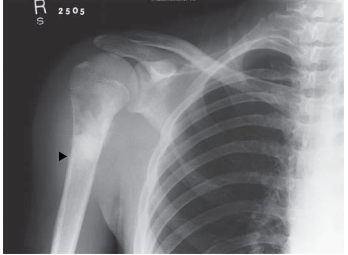
Figure 54.1 Naomi’s shoulder X-ray
Questions
• What is the diagnosis?
• What is the management?
The diagnosis is an osteosarcoma of the right humerus. There is no differential. This is a malignant tumour that classically presents in adolescence and often comes to light after a relatively minor injury. It is still not uncommon for there to be a delay in diagnosis because it is rare and not considered in the differential diagnosis of limb and joint pain. The characteristic features on the X-ray are:
• bone destruction
• gross swelling
• elevation of the periosteum with creation of Codman’s triangle (marked with an arrow on the X-ray)
• ‘sunray’ spicules of new bone visible in the muscle and subcutaneous tissues. The first step is regular adequate pain relief. Non-steroidal anti-inflammatory agents may be adequate but it is highly likely that opioids will be needed. This is an aggressive tumour with rapid expansion of the periosteum which is exquisitely painful. Secondly, a senior paediatrician – preferably from the local ‘shared care’ oncology team – should break the news to the girl and her family. They will be devastated and quite possibly angry at the perceived delay in diagnosis. The local team will have the experience and knowledge to answer any immediate questions. They will also know that the best route for onward referral is to a specialist paediatric oncology centre and not, at this stage, to orthopaedics. Although a tissue diagnosis is required, she needs to be screened for metastases as this may alter the management significantly. Osteosarcomas usually spread to lung and bone and she will need a chest CT scan and a bone scan plus an MRI scan of the shoulder to guide future surgery. The biopsy should only be taken in a specialist centre (or with their explicit agreement) and reviewed by a team of specialist histopathologists. The specific management of osteosarcoma is initial chemotherapy to reduce tumour bulk and to clear any metastases, followed by surgery followed by further chemotherapy. Definitive surgery is probably contraindicated if metastases have not cleared or significantly reduced with initial chemotherapy, although some patients with isolated lung secondaries do extremely well following their resection. Modern surgery is largely successful at avoiding mutilating amputation using prostheses that can be externally ‘lengthened’ as the patient grows. Prognosis depends upon the presence of metastatic spread at presentation – bone secondaries carry a particularly grave outlook – and on response to chemotherapy as evidenced by tumour necrosis at surgical resection. More than 90 per cent necrosis is associated with an improved outcome. Overall prognosis is a 5-year survival rate of approximately 60 per cent.
KEY POINTS
• Children do not get ‘frozen shoulder’ and functional pain is a diagnosis of exclusion.
• Bone tumours are rare but should be considered in any patient with unexpectedly severe symptoms following a minor injury.
• The care of children with cancer should be coordinated by a specialist centre.
• Centralization of care, entry into randomized controlled trials and the use of national or international protocols have steadily improved the prognosis in childhood cancer.
need an explanation for this answer? contact us directly to get an explanation for this answer