AN INFANT WITH POOR WEIGHT GAIN
History Tommy is a 9-month-old boy who is referred to the outpatient clinic with failure to thrive. His birth weight was 3.17 kg, he gained weight well initially and was weaned at 6 months. His appetite has been poor over the last couple of months and his mother describes him as miserable. He has no vomiting and opens his bowels four times a day. The stool is loose and smelly but contains no blood or mucus. His mother breast-fed until 4 months of age. The family have recently returned from Turkey but his mother states that the poor feeding and weight loss preceded their holiday. His father has Crohn’s disease, for which he has required several operations.
Examination Tommy is a thin, pale-looking infant. He is miserable and cries easily, and his abdomen is distended. There are no signs of tenderness, masses or organomegaly. The oral cavity and perianal area appear normal. There are no other signs. His centile chart is in Figure 30.1.
INVESTIGATIONS
Normal
Haemoglobin 8.2 g/dL 9.0–14.0 g/dL
Mean cell volume 68 fL 70–86 fL
White cell count 9.8 109/L 4.0–11.0 109/L
Platelets 432 109/L 150–400 109/L
C-reactive protein 9 mg/L 6 mg/L
Ferritin 6 ng/ml 15–200 ng/ml
Urea and electrolytes Normal
Liver function tests Normal
Bone chemistry Normal
Immunoglobulins Normal
Coeliac screen
Transglutaminase IgA Antibody 100 U/mL 0–8 U/mL
Urine dip Negative
Stool – no bacterial growth, no ova, cysts or parasites
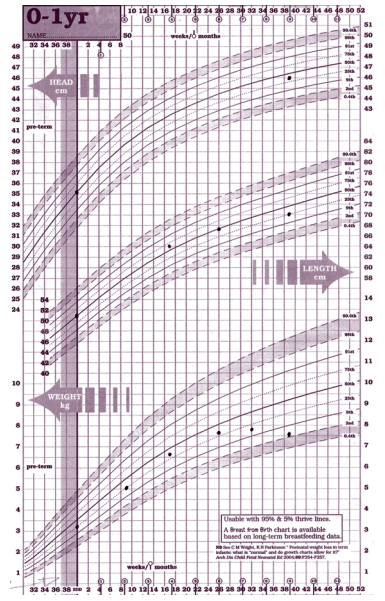
Figure 30.1 Centile chart. (Chart reproduced with kind permission of the Child Growth Foundation.)
Questions
• What is the definition of failure to thrive?
• What are the causes of failure to thrive?
• What is the likely diagnosis and how could it be confirmed?
Failure to thrive is a descriptive term and not a diagnosis. It is often defined as a weight, or a rate of weight gain, that is significantly below what is normal for a child of that age and sex. Some authors define failure to thrive as a weight that has fallen two centile lines on the standard growth charts. Although this term can refer to height as well as weight, it is usually used in relation to weight in children under 2 years of age.
Causes of failure to thrive
Inadequate intake of food
• Poor feeding
• Mechanical problem such as a cleft palate or bulbar palsy
Malabsorption
• Coeliac disease
• Cystic fibrosis
Excessive loss of nutrients
• Vomiting due to gastro-oesophageal reflux
• Protein-losing enteropathy, e.g. cow’s milk protein
intolerance Increased nutrient requirement
• Congestive cardiac failure
• Chronic infection, e.g. HIV
Miscellaneous causes
• Dysmorphic syndromes, e.g. Russell–Silver syndrome
• Inborn errors of metabolism
Psychosocial
• Child abuse and neglect
• Emotional and social deprivation
It is important to take a full dietary history. The commonest cause of failure to thrive is a poor nutrient intake which may be due to feeding mismanagement or psychosocial problems. Failure to thrive may also be the result of a combination of the factors in the above box, and in some cases no cause is found. Crohn’s disease is very rare in this age group and the father’s illness is coincidental. The likely diagnosis is coeliac disease. Steatorrhoea (with pale, greasy, smelly stool) and diarrhoea are typical. The abdominal distension is due to distension of the intestinal loops with fluids and gas. The centile chart shows that the weight has crossed two centile lines since 6 months and that there has also been weight loss. This would correspond with weaning at 6 months and the introduction of gluten in wheat and other foods. The anaemia is secondary to the poor nutrient intake and malabsorption. Folate as well as iron deficiency may occur. Anti-tissue transglutaminase is 95 per cent accurate in diagnosing coeliac disease (it is important to simultaneously measure IgA, as anti-tissue transglutaminase is an IgA antibody and IgA deficiency would invalidate the test). However, the definitive diagnosis is based on an endoscopy with a jejunal biopsy. In cases of coeliac disease, there is subtotal villous atrophy, crypt hypertrophy and a lamina propria plasma cell infiltrate. Treatment is with a gluten-free diet
KEY POINTS
• The commonest cause of failure to thrive is a poor nutrient intake.
• Serological testing is very useful in the diagnosis of coeliac disease, but definitive diagnosis is with a jejunal biopsy.
• Treatment of coeliac disease is with a gluten-free diet.
need an explanation for this answer? contact us directly to get an explanation for this answer