A BOY WITH BOW LEGS
History
Tariq is a 2-year-old Asian boy who presents to paediatric outpatients with bow legs and poor weight gain. He was born in Bangladesh and the family moved to the UK when he was 3 months old. He was breast-fed for the first year. His mother states that he currently has several bottles of cow’s milk a day and that he has a poor appetite with a poor intake of solids. He has no gastrointestinal symptoms. His mother feels that he is not as active as other boys his age. There is no history of fractures. There is no family history of note.
Examination
His is pale, with a prominent forehead and a marked bow leg deformity. He has swollen wrists (see X-ray in Fig. 22.1) and ankles. There are no other clinical signs. His height is on the 25th centile, and his weight is on the 2nd centile.
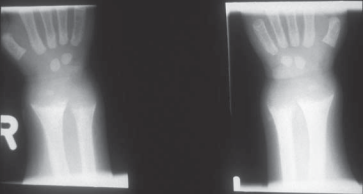
Figure 22.1 Tariq’s wrist X-ray.
INVESTIGATIONS
Normal
Haemoglobin 9.8 g/dL 11.5–15.5 g/dL
Mean cell volume 64 fL 70–86 fL
Mean corpuscular haemoglobin 22 pg 24–30 pg
White cell count 8.7 109/L 4.0–11.0 109/L
Platelets 572 109/L 150–400 109/L
Ferritin 4 ng/mL 15–200 ng/mL
Haemoglobinopathy screen Normal
Sodium 137 mmol/L 135–145 mmol/L
Potassium 4.1 mmol/L 3.5–5.0 mmol/L
Urea 4.7 mmol/L 1.8–6.4 mmol/L
Creatinine 60 µmol/L 27–62 µmol/L
Calcium 2.21 mmol/L 2.20–2.70 mmol/L
Phosphorous 1.30 mmol/L 1.25–2.10 mmol/L
Alkaline phosphatase (ALP) 1372 U/L 145–420 U/L
Bilirubin 16 µmol/L 2–26 µmol/L
Alanine aminotransferase (ALT) 32 U/L 10–40 U/L
Questions
• Name the two disorders that affect this child.
• What is the treatment?
This type of nutritional history in an Asian child, the accompanying clinical signs, the high ALP, the borderline calcium and the wrist X-ray all point to rickets. Furthermore, the poor nutritional intake, the pallor and the microcytic hypochromic anaemia are typical of iron deficiency anaemia. Rickets is a disorder characterized by a failure in the mineralization of growing bones. The majority of cases are due to inadequate sunlight exposure coupled with nutritional deficiency. The condition is more common in dark-skinned infants who need greater sun exposure to synthesize adequate amounts of vitamin D. Prolonged breast-feeding increases the risk of rickets as breast milk is a poor source of vitamin D. Infant formulas are often supplemented with vitamin D, but cow’s milk is also a poor source of vitamin D. Diseases that interfere with the metabolic conversion and activation of vitamin D, such as severe renal and liver disease, can lead to rickets. Illnesses associated with malabsorption, such as coeliac disease, can also lead to rickets. Other diseases that interfere with calcium and phosphorus homeostasis can cause rickets, e.g. renal tubular defects, such as hypophosphataemic rickets, in which there is failure of phosphate absorption, or Fanconi’s syndrome in which there is a defect in the reabsorption of phosphate, glucose and amino acids. Clinical features include swollen wrists and ankles, frontal bossing, prominent costochondral junctions (a rickety rosary), bow legs or knock-knees, craniotabes, muscle weakness, tetany and hypocalcaemic fits. The radiograph demonstrates the typical appearance in rickets with widening of the growth plate and cupping, splaying and fraying of the metaphysis. A vitamin D level to confirm the nutritional aetiology of the rickets and antitransglutaminase antibody levels to rule out coeliac disease would be helpful. Iron deficiency anaemia is said to occur in a quarter of children under 5 years of age. Cow’s milk is a poor source of iron. Although usually nutritional, blood loss should be considered as a possible cause, especially in older children. This may be due to occult gastrointestinal blood loss secondary to a peptic ulcer, a Meckel’s diverticulum or inflammatory bowel disease. A ferritin level should be done to confirm the diagnosis and is likely to be very low. A haemoglobinopathy screen should be performed in high-risk groups to exclude disorders such as thalassaemia that can also cause a microcytic hypochromic anaemia and that may coexist with iron deficiency. Infants may be pale, tired, irritable and anorexic. In severe cases they can be tachypnoeic. There is evidence that iron deficiency anaemia can also have adverse effects on attention span and learning. Treatment consists of a 3-month course of high-dose oral vitamin D. Bone chemistry should be measured 2 weeks after starting treatment and regularly thereafter to avoid hypercalcaemia and to ensure that the biochemical and haematological parameters normalize. This should be followed by maintenance doses of vitamin D for the long term. The prognosis for complete resolution of the deformities is good. In cases where the serum calcium is low, calcium is also given initially until levels normalize. There is often an accompanying iron deficiency anaemia, as in this case. Red meat and green vegetables are good sources of iron and some foods, such as cereals, are often fortified with iron. The anaemia should be treated with a 3-month course of oral iron.
A dietetic referral and screening of the siblings for rickets and iron deficiency would also be advisable.
KEY POINTS
• Rickets is usually secondary to inadequate exposure to sunlight and poor nutrition.
• Swollen wrists, a rickety rosary and bow legs are typical clinical features.
• Treatment is with vitamin D.
• Iron deficiency is very common in young children and can be successfully treated with dietary advice and oral iron.
need an explanation for this answer? contact us directly to get an explanation for this answer