A GIRL WITH EARLY PUBERTY
History
Tracey is a 6.5-year-old Afro-Caribbean girl who presents to the paediatric clinic with a 1-year history of breast development and a 9-month history of pubic and axillary hair. She sweats more than previously and has body odour. She has no acne. Her periods have not started. Her mother feels that she has been growing taller at a faster rate in the past year. She has headaches but these occur less than once a month and are not severe. She has no visual problems. Her mother had her menarche at the age of 13 years. There is no past medical history of note.
Examination
Her breasts are Tanner stage 3, and her pubic hair Tanner stage 2 (see p. 60). There is sparse axillary hair. There are no neurological signs and no abdominal masses or organomegaly. Her height, at 133 cm, is just over the 99.6th centile and her weight, at 27 kg, is on the 91st centile (mid-parental height between 50th and 75th centile).
INVESTIGATIONS
Oestradiol – 172 pmol/L (prepubertal value 50)
Luteinizing hormone-releasing hormone (LHRH) test
Time (min) Luteinizing hormone Follicle-stimulating hormone
(LH, units/L) (FSH, units/L)
0 3.8 3.0
30 14.2 7.3
60 36.4 12.6
Pelvic ultrasound – bilaterally enlarged ovaries with multiple small follicular cysts, the largest being 7 mm in diameter.
The uterus is enlarged for age.
There is no endometrial stripe
Bone age – 9.5 years
Cranial MRI – see Figure 18.1
Figure 18.1 Cranial MRI. (Reproduced with permission from Raine JE, Donaldson MDC, Gregory JW et al., Practical Endocrinology and Diabetes in Children, Blackwell Science, 2006.)
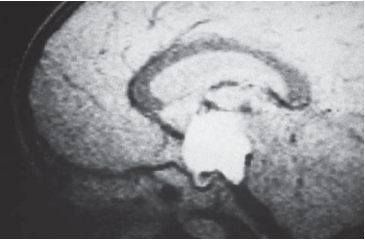
Figure 18.1 Cranial MRI. (Reproduced with permission from Raine JE, Donaldson MDC, Gregory JW et al., Practical Endocrinology and Diabetes in Children, Blackwell Science, 2006.)
Questions
• What is the precise diagnosis?
• What is the treatment?
Tracey has gonadotrophin-dependent precocious puberty secondary to a hypothalamic hamartoma. This condition differs from gonadotrophin-independent precocious puberty, which is caused by the abnormal secretion of sex steroids independent of the hypothalamopituitary axis. Precocious puberty is defined in the UK as puberty commencing before the age of 8 years in females and 9 years in males. In the United States these criteria have been recently revised to below 7 years in a Caucasian girl and below 6 years in an Afro-Caribbean girl. There may be a family history. The first sign of puberty in girls is breast development, and in boys is testicular enlargement with a testicular volume of 4 mL denoting the start of puberty. Tracey’s puberty started at 5 years and 6 months. Sweating, body odour, acne and a height spurt (height velocity increases from 5 cm/year prepubertally to as much as 12 cm/ year) are all part of puberty. The high height centile relative to the mid-parental centile and the advanced bone age all support early puberty. The LHRH test can help diagnose gonadotrophin-dependent precocious puberty. An LH value 8 units/L with a predominant LH response is diagnostic. The ultrasound is also in keeping with puberty. In the majority of girls ( 90 per cent) the cause is idiopathic. The earlier the onset of puberty, the greater the likelihood of there being a cause. Investigation should be considered in all girls below 8 years of age. The presence of neurological features should also prompt investigations, including a cranial MRI. In a minority of girls, a hypothalamic hamartoma can lead to early puberty. Rarely, malignant brain tumours can cause precocious puberty. Acquired neurological injuries, such as encephalitis, hydrocephalus and radiation, can also lead to early puberty. In contrast, in boys early puberty is usually secondary to a cranial lesion and MRI scanning is mandatory. Treatment is with monthly injections of an LHRH analogue. This should halt puberty and may lead to some regression. Although currently tall, this girl is at risk of premature fusion of her epiphysis with a short adult height. Psychosocial considerations are also an important indication for treatment. Coping with the emotional changes of puberty and possible early menarche is difficult in young girls. In girls with mild, slowly progressive early puberty, no treatment may be necessary. In boys, treatment is also with an LHRH analogue. Any underlying lesion should be treated. Treatment is often continued until 11 years of age. Hypothalamic hamartomas are benign and often remain static in size or grow slowly, producing no other signs. Neurosurgical intervention is not indicated except in rare patients with intractable seizures.
KEY POINTS
• Precocious puberty is defined as puberty starting below the age of 8 years in girls and 9 years in boys.
• In females it is usually idiopathic, but in males it is usually secondary to a cranial lesion.
• Treatment is with LHRH analogues (any underlying lesion may also need treatment)
need an explanation for this answer? contact us directly to get an explanation for this answer