RECURRENT CHEST INFECTIONS
History
Conor is a 4-year-old boy who is admitted to the paediatric ward from the A&E department with pneumonia. This is his fourth hospital admission. In the first year of life, he was admitted twice with bronchiolitis, requiring several days on oxygen, and about 6 months ago he was admitted with pneumonia, again requiring oxygen and intravenous antibiotics. He has had many courses of oral antibiotics over the last few years from his GP for chest infections. He also has recurrent abdominal pain and his parents report large offensive stools. His parents both smoke 20–30 cigarettes/day. He is unimmunized as his parents are worried about potential side-effects.
Examination
He is small (height ninth centile, weight second centile), pale-looking, miserable and very clingy to his mother. He has finger clubbing. His temperature is 38.7C, respiratory rate 40 breaths/min, heart rate 140 beats/min and oxygen saturation 89 per cent in air (95 per cent in facemask oxygen). There is reduced air entry at the left base with bronchial breath sounds in the left midzone, and coarse crackles are heard on both sides of the chest. Cardiovascular examination is unremarkable. His abdomen is mildly distended but non-tender.
INVESTIGATIONS
Haemoglobin 10.1 g/dL 11.0–13.8 g/dL
White cell count 19.7 109/L 6–17 109/L
Platelets 401 109/L 210–490 109/L
Immunoglobulin G 10.2 g/L 5.0–15.0 g/L
Immunoglobulin A 2.5 g/L 0.3–3.0 g/L
Immunoglobulin M 1.8 g/L 0.4–2.0 g/L
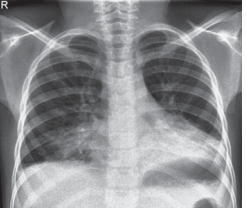
Chest radiograph – see Figure 5.1
Questions
• What does the chest radiograph show?
• What is the likely underlying diagnosis?
• What investigation would you do to confirm the diagnosis?
• What are the other manifestations of this disease?
The chest radiograph shows consolidation with some collapse of the left lower lobe and further consolidation in the right middle lobe. There are small bilateral pleural effusions. These features are consistent with the clinical diagnosis of pneumonia. The combination of clubbing and recurrent chest infections is strongly suggestive of cystic fibrosis (CF). This is the commonest cause of clubbing in children in the UK. Normal immunoglobulins exclude antibody deficiencies such as X-linked hypogammaglobulinaemia. Malabsorption (with bulky, offensive stools) is another common feature of CF. Cystic fibrosis is an autosomal recessive condition affecting 1 in 2500 children born in the UK. It is the commonest autosomal recessive disorder in the Caucasian population. Cystic fibrosis is caused by defects in the gene for the CF transmembrane conductance regulator (CFTR). This gene encodes for a protein that functions as a chloride channel and is regulated by cyclic AMP. Cystic fibrosis causes dysfunction of multiple organs – most prominently lung, intestine, pancreas and liver. Clinical phenotypes of CF can be very variable, affecting the age at presentation, symptoms and the severity of different organ involvement. Thus CF should be considered in any of the situations listed below.
Presentations of cystic fibrosis
Neonatal
• Meconium ileus
• Intestinal atresia
• Hepatitis/prolonged jaundice
Infant
• Rectal prolapse (may be recurrent)
• Failure to thrive
• Malabsorption and vitamin deficiency (A, D, E, K)
Older children
• Recurrent chest infections
• ‘Difficult’ asthma • Haemoptysis
• Nasal polyps
• Distal intestinal obstruction syndrome
• Liver disease
• Diabetes mellitus
Diagnosis can be made by the sweat test, which will demonstrate elevated sweat sodium and chloride concentrations, and by genetic testing. National newborn screening using blood spots collected on day 5 of life are now tested for immunoreactive trypsinogen (at the same time as testing for phenylketonuria, congenital hypothyroidism and sickle cell disease). This is now leading to the identification of cases before the onset of clinical disease. Once a child is diagnosed with CF, he or she will need multidisciplinary team management under the supervision of a paediatric respiratory consultant. Optimal care will aim to maintain lung function by treating respiratory infections and removing mucus from the airways with physiotherapy, and to maintain adequate growth and nutrition with pancreatic enzyme and nutritional supplements.
KEY POINTS
• Cystic fibrosis should be considered in children with recurrent chest infections or malabsorption.
• Cystic fibrosis is the commonest cause of finger clubbing in children.
need an explanation for this answer? contact us directly to get an explanation for this answer